If the patient is pregnant, contact obstetric team
see VTE – Pulmonary embolism guideline in Obstetric guidelines
see VTE – Pulmonary embolism guideline in Obstetric guidelines
DEFINITION
- Haemodynamically stable PE with a systolic BP ≥90 mmHg
- PE range from small with normal BP to large with borderline BP and right ventricular dysfunction
- If patient becomes haemodynamically unstable during management, follow PE: Unstable guideline
RECOGNITION
- Pulmonary venous thromboembolism (PE) is often missed clinically, particularly in:
- severe cardiorespiratory disease
- elderly patients
- Suspect the diagnosis in any patient who does not respond to initial therapy, or in whose condition there has been an unexplained deterioration
- Most episodes follow popliteal or iliofemoral DVT
Symptoms
- Small emboli present with dyspnoea
- Moderate-sized emboli present with signs of infarction and pleuritic pain
- Dyspnoea (present in 90% of cases) – may be of sudden onset
- Pleuritic chest pain
- Haemoptysis
- Syncope
Signs
- Tachypnoea (>20 breaths/min)
- Fever
- Pleural rub
- Tachycardia
- Maybe absent
Differential diagnosis
- Pneumonia
- Myocardial infarction (MI)
- Exacerbations of asthma and COPD
INVESTIGATIONS
- FBC, INR, APTT and U&E
ECG and CXR
- ECG and CXR are often normal
- not to be used to confirm/refute the diagnosis
- useful for identifying other diseases and explaining symptoms
- ECG may show:
- sinus tachycardia, an S1 Q3 T3 pattern
- right bundle branch block, P pulmonale or right axis deviation
- Chest X-ray may show:
- non-specific shadows or a raised hemidiaphragm
- pulmonary oligaemia, linear atelectasis or small pleural effusion
Ordering D-dimer, perfusion scan or CTPA?
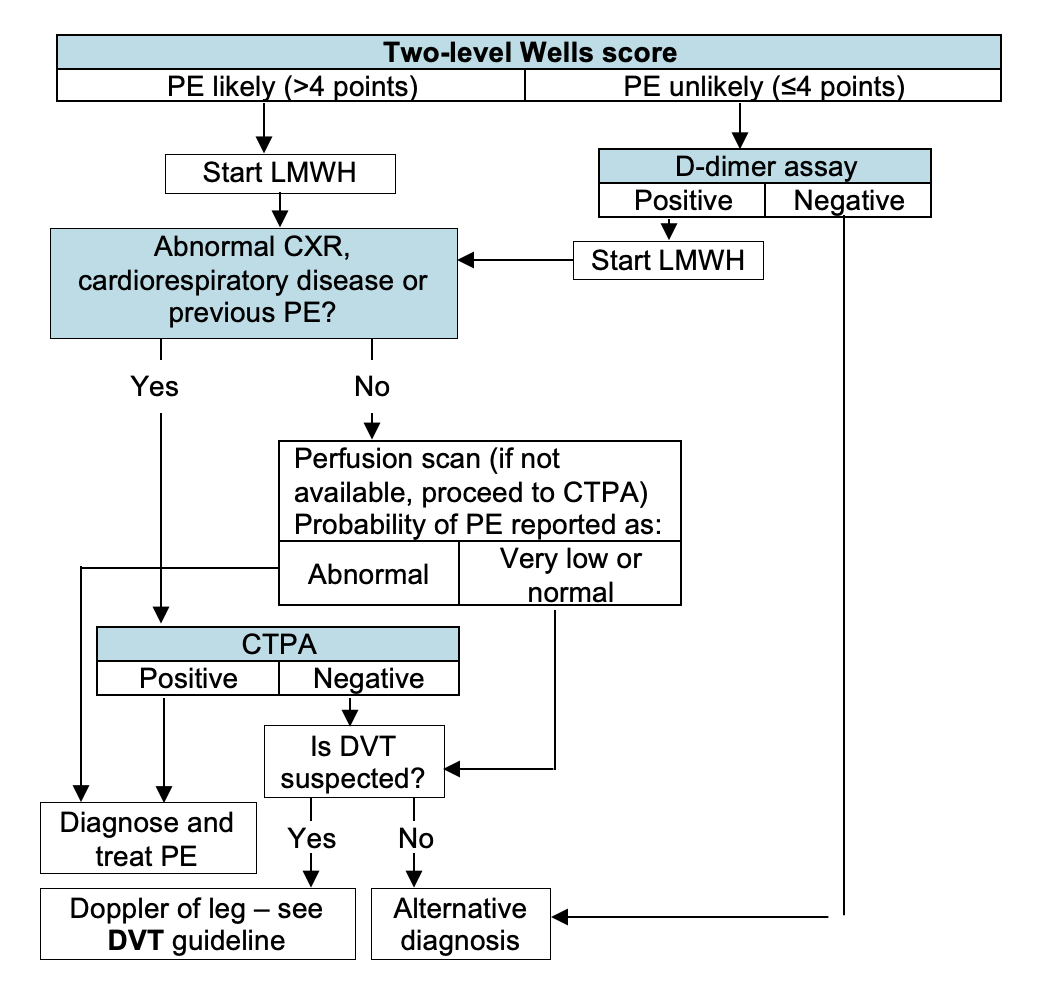
- Order test indicated by two-level PE Wells score, clinical status and chest x-ray results
Select which of the following clinical features the patient has:
PE Likely: appropriate test to order
- Order CTPA
- Order perfusion scan (if not available, order CTPA)
D-dimer
- Raised in many clinical states
- do not request if clinical probability of PE is high, in probable massive PE or where an alternative diagnosis is highly likely
- normal D-dimer concentration virtually rules out thrombosis
Leg Doppler ultrasound
- Alternative to lung imaging in patients with clinical DVT
ASSESSMENT
- Follow selectors below or flowchart (equivalent)
- Choose result of test indicated by two-level PE Wells score, clinical status and chest x-ray results
CTPA result
Perfusion scan
D-dimer
IMMEDIATE MANAGEMENT
General
- Oxygen – see Treatment of hypoxaemia guideline
- Adequate analgesia for pleuritic pain – paracetamol alone is unlikely to be adequate
- if well hydrated and eGFR ≥30 mL/min, ibuprofen 400 mg oral 8-hrly
- in dehydrated patient or if eGFR <30 mL/min, to prevent renal damage, prefer morphine sulphate 10 mg oral 4-hrly – ibuprofen may be substituted once adequate fluid replacement achieved if eGFR ≥30 mL/min
- if patient pregnant, prefer morphine sulphate 10 mg oral 4-hrly
- if patient taking ACE inhibitor avoid NSAIDS, including ibuprofen
- A high right atrial pressure (i.e. ↑JVP) is common and does not need to be treated
- AVOID diuretics
Specific
- Commence dalteparin as soon as PE suspected – see Dalteparin for VTE guideline
- if anticoagulation contraindicated, consultant physician, staff physician must decide which carries most risk – complications of therapy (consider a vena caval filter) or the DVT
Inferior vena caval filter (IVCF)
- Temporary IVCF can be used if patient:
- cannot have anticoagulation treatment, which will need to be removed when patient becomes eligible for anticoagulation therapy
- recurrent VTE despite increasing INR target range to 3–4 or trial of Dalteparin – discuss with haematology
- ensure strategy for removing IVCF at earliest possible opportunity is planned and documented
SUBSEQUENT MANAGEMENT
Assess suitability for ambulatory care
- Assess patients by sPESI risk score and exclusion criteria
Determine Simplified Pulmonary Embolism Severity Index (sPESI)
Check exclusion criteria
Decision
- If sPESI is high risk or an exclusion criterion, manage as inpatient
- consider for early discharge when low risk score
- If SPESI is low risk and no exclusion criterion, manage as ambulatory care
Suitable for ambulatory care of PE
- Refer to AMU or ambulatory emergency care centre (AEC)
- Provide patient information on:
- signs and symptoms of recurrence, major bleeding and additional complications
- AMU and AEC contact details in event of complications and concerns
- Complete the PE Ambulatory proforma
- Arrange review in AEC within a week of discharge
- Refer to respiratory clinic
MONITORING ON WARD
- Daily clinical examination for signs of further embolism, right heart failure, and secondary infection of a pulmonary infarct
Monitoring dalteparin treatment
- See Dalteparin for VTE guideline
Inferior vena caval filter (IVCF)
- Temporary IVCF can be used if patient:
- cannot have anticoagulation treatment, which will need to be removed when patient becomes eligible for anticoagulation therapy
- recurrent VTE despite increasing INR target range to 3–4 or trial of dalteparin – discuss with haematology
- ensure strategy for removing IVCF at earliest possible opportunity is planned and documented
Maintenance anticoagulation
- Start warfarin as soon as diagnosis confirmed – see Warfarin guidelines
- Continue Dalteparin (see Dalteparin for VTE guideline) for a minimum of 5 days until:
- INR established within therapeutic range 2–3 (3–4 for recurrent DVT occurring while INR within the range 2–3) for at least 2 consecutive days
- If patient injection drug user or has active cancer, consider continuing therapeutic dalteparin treatment, rather than converting to warfarin
- If APTT ratio exceeds 2.5 in a patient being given unfractionated heparin
- INR may be elevated by heparin
- do not use INR as a guide to adjustment of warfarin dosage
Rivaroxaban
- If LMWH or warfarin not suitable, consider rivaroxaban, particularly if:
- previous intracranial bleed
- ≥12 months anticoagulant therapy is required
- anticipated difficulties with INR monitoring and understanding dose adjustments
- needle phobia
- other comorbidities (e.g. deranged LFT, excessive alcohol intake) increasing risk of bleeding on warfarin. Discuss with haematologist
- Contraindicated if eGFR <15 mL/min, in pregnancy and if breastfeeding
Dosage and monitoring
- 15 mg 12-hrly oral for first 3 weeks, 20 mg daily oral thereafter for duration of therapy
- No monitoring is required
- If 15mL/min < eGFR <50 mL/min, reduce dose as per BNF – discuss with haematologist
Screen for cancer
- In all patients with a confirmed PE, Chest X-ray, FBC, LFT, calcium and urinalysis
- If patient aged >40 yr has first unprovoked PE, consider performing:
- a thoraco-abdominal–pelvic or abdominal-pelvic (discuss with radiology) CT scan
- for women, a mammogram
Screen for thrombophilia
- If patient aged <45 yr with unprovoked PE, discuss screening for inherited or acquired thrombophilia with haematology consultant
DISCHARGE AND FOLLOW-UP
- Ensure INR in appropriate range and stable
Duration of anticoagulation
- After a first provoked thromboembolic event, continue warfarin for 3 months
- Continue indefinitely for life-threatening PE
- For recurrent or unprovoked PE discuss with haematology and/or respiratory physician
- If patient has active cancer, reassess risks and benefits of continuing anticoagulation at 6 months
Outpatient investigations
- If evidence of right ventricular dysfunction or raised Troponin or BNP biomarkers, arrange echocardiogram
- arrange follow-up for result in 10-12 weeks for respiratory clinic
Advice to patient
- Advise patient that many drugs (including alcohol) interact with warfarin
- To remind their GP, if additional medication is prescribed, that they are taking warfarin
- Give patient a yellow anticoagulation therapy record booklet in which the following information has been entered:
- indication for warfarin, target INR
- start date and duration of therapy
- the last 4 INR results and date of next INR
Monitoring
- Refer to anticoagulant management service for follow-up appointment date
- Ensure discharge letter includes diagnosis, dosage of warfarin and date of clinic appointment
- If anticoagulation to be monitored by GP, supply GP with written information (on separate sheet, stapled to discharge letter) about:
- indication for anticoagulation
- proposed duration of treatment
- proposed target range for INR
- details of anticoagulation in hospital (give dates, INR results and dosage taken)
Document
- Document in medical record
- patient has been given written and verbal information about warfarin and has been referred to anticoagulation clinic
- duration of treatment
- outpatient investigations
- monitoring arrangements