Alert haematology to all admissions
VASO-OCCLUSIVE CRISIS
Symptoms and signs
- Severe pain (usually in extremities, back or abdomen)
- Dehydration
- Enlarged liver or spleen
- Bone pain
- Low grade fever (<38°C) even in absence of infection
History
- Is pain similar to that of a sickle cell crisis or is it different in any way?
- Analgesia already taken for current episode?
- Any precipitating factors – infections, dehydration, stress?
- Any complicating factors:
- shortness of breath/cough/chest pain
- headache/neurological symptoms
- abdominal pain/priapism
- features to indicate infection
- assess features of other non sickle related presentations
- Previous episodes and complications
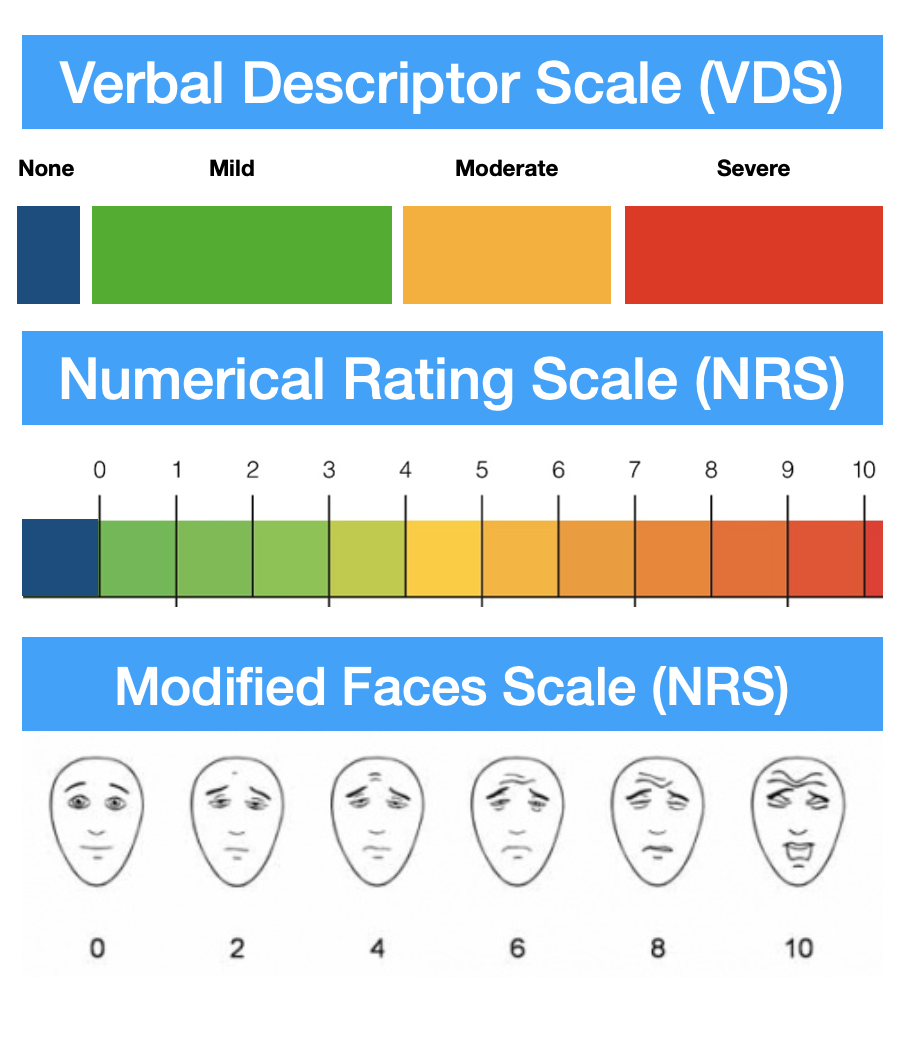
- Use age-appropriate pain score
Examination
- Look for:
- tachycardia
- tachypnoea
- hypo and hypertension
- fever
- dehydration
- SpO2 on air and on oxygen (target oxygen saturation 95%)
- chest signs
- hepatosplenomegaly
- If neurological symptoms, full neurological findings
Investigations
- Presence of sickle cells in blood film does not correlate with clinical events
- FBC and reticulocyte count
- check whether Hb and reticulocyte count similar to patient’s baseline
- worsening anaemia and low reticulocyte count may indicate virus (parvovirus) – induced bone marrow aplasia
- Group and save
- in new patients, obtain full red cell phenotype
- U&E, LFT
- If fever or relevant symptoms or signs, septic screen
- Only if infection or acute chest syndrome suspected (see below), CXR
- Painful bones need not normally be X-rayed
IMMEDIATE TREATMENT
Analgesia
- Select pain assessment tool (PAT)
- Administer first dose of analgesia within 30 min of presentation to emergency department
- Ensure drug, dose and administration route are suitable for severity of pain and age of patient
- Refer to patient’s individual care plan if available
- Offer a bolus of strong opioid to all patients presenting with:
- severe pain
- moderate pain not relieved by analgesia already taken
Non-opioid analgesia
- Not all patients require opioid analgesia although many do
- If no contraindications, offer the following regularly:
- paracetamol 1 g oral 6-hrly
- if well hydrated and eGFR ≥30 mL/min, naproxen 250 mg oral 6-hrly or ibuprofen 400 mg oral 8-hrly
- dihydrocodeine 30–60 mg oral 4–6 hrly (max 240 mg in 24 hr)
- Review doses in presence of renal impairment
- Do not use pethidine for treating pain in an acute sickle cell episode
Opioids in opioid naïve patients
- If weight ≤50 kg, morphine 2.5 mg SC up to every 2 hr
- If weight >50 kg, morphine 5 mg SC up to every 2 hr
Opioids in patients using opiates/opioids regularly
- May require higher doses
- e.g. morphine 5–10 mg SC up to every 2 hr or equivalent dose of diamorphine or other alternatives
- if patient prefers and usually uses IV morphine, give morphine 0.1 – 0.15 mg/kg IV (maximum 10 mg) over 5 min
- pethidine is no longer recommended for sickle vaso-occlusive pain
Monitoring
- Reassess response in approximately 15–30 min after the completion of the IV infusion, or 30–60 min after SC injection
- consider repeating/increasing dosage according to efficacy
- do not adjust the dose of morphine before the expected time of peak onset of pain relief (i.e. 20 min for IV dosing)
- Assess pain every 30 min until satisfactory relief then monitor at least every 4 hr using an age-appropriate pain assessment tool
- if patient has severe pain on reassessment, offer second bolus dose of a strong opioid
- If repeated bolus doses of a strong opioid are needed within 2 hr
- consider admission to a surgical ward for patient-controlled analgesia – see Patient-controlled analgesia guideline in the Surgical guidelines
- Monitor patients receiving at least hourly for presence of adverse effects
- including respiratory depression (sedation score, respiratory rate) – see Opioids: monitoring and dose adjustment guideline in the Surgical guidelines
Itch and nausea
- Non-sedating antihistamines for itch
- Ondansetron for nausea
Fluid replacement
- Replace fluid orally if possible
- Venous access often difficult in patients with SCD:
- reserve for situations where oral intake inadequate or inappropriate (e.g. vomiting)
- If unable to give orally, glucose (4%) and sodium chloride (0.18%) 1 L by IV infusion over 3 hr
- then follow IV fluid maintenance guideline
- NEVER add potassium chloride to infusion bags
- Avoid using veins in ankles/feet for venous access
- cannulation carries high risk of leg ulceration
- Avoid central lines as they carry high complication rate
Blood transfusion
- Indications for blood transfusion in sickle cell disease are very specific
- discuss all cases with haematologist
Oxygen therapy
- If SpO2 <94%, give oxygen. See Oxygen therapy in acutely hypoxaemic patients guideline
- Carry out a full assessment of the reason for hypoxia
- opiate-induced respiratory suppression
- severe chest infection
- chest syndrome (see below)
- If SpO2 cannot be maintained >94%, discuss with critical care team and haematology team
Antimicrobials
- Continue prophylactic antimicrobials as recommended by patient’s haematologist
- see BNF if not already on prophylaxis
- If evidence of infection, give antimicrobials
- see appropriate guideline for type of infection
Thromboprophylaxis
- Unless contraindicated, give thromboprophylaxis
- see Prophylaxis against venous thromboembolism guideline
SUBSEQUENT MANAGEMENT
- Painful crises usually last about 1 week
- Once pain controlled, reassess analgesic regimen daily and taper dosage gradually
- change to oral morphine (1 mg SC diamorphine = 3 mg oral morphine)
- If Hb falls below 50 g/L, especially if reticulocyte count decreased, consider blood transfusion
- discuss with haematologist
MONITORING TREATMENT
- Respiratory rate hourly after opioid started for evidence of respiratory suppression
- Pulse oximetry
- Fluid balance
- U&E for dilutional hyponatraemia
- Consider PAT to record pain response to analgesia
OTHER COMPLICATIONS
- Discuss with haematologist
Acute chest syndrome
- Acute life-threatening complication of sickle cell disease
- breathlessness, hypoxia, fever and new onset pulmonary infiltrates in CXR
- Discuss urgently with haematologist
Priapism
- Painful prolonged erection with/without prior sexual stimulus
- This is an emergency
- involve urologist early as penile aspiration/irrigation may be necessary
- in some instances shunt procedures are needed
Stroke
- More common in children
- Ischaemic stroke is more common in children
- Haemorrhagic stroke is more common in adults
Investigations
- Emergency CT scan of head to confirm whether ischaemic or haemorrhagic
- MRI scan of brain to delineate area of ischaemia/haemorrhage
- Carotid Doppler ultrasound scan
- Urgent review by neurologist and haematologist for exchange transfusion to reduce HbS <30%
Splenic sequestration
- More common in infants and children
- Often associated with sepsis
- Clinical features:
- rapidly enlarging, painful spleen
- anaemia – may present with shock
- fall in Hb of 20 g/L from baseline
Management
- Resuscitate and treat shock
- Emergency (top-up) transfusion: to baseline Hb
- Broad spectrum antimicrobials to cover pneumococcus and haemophilus
Hepatic sequestration
- Acute tender hepatomegaly and anaemia
- manage with a top-up transfusion to baseline Hb
Gallstone complications
- Common in this patient population
- manage as any other patient
Aplastic crisis
- Transient arrest of erythropoiesis
- Abrupt reduction in haemoglobin concentration
- Associated with human parvovirus B19, streptococci, salmonella, streptococci, and Epstein-Barr virus infections
- Emergency (top-up) transfusion: to baseline Hb
- Reticulocytes typically reappear within 2–14 days
Osteomyelitis
- Increased incidence in SCD from infection of infarcted bone
- Usually due to salmonella or other gram-negative organisms, such as Escherichia coli but also Streptococcus pneumoniae, Haemophilus influenzae, and Staphylococcus aureus
- Clinical presentation is often similar to a VOC frequently plus:
- a prolonged duration of fever and pain
- swelling and pain that is localised to a single site
- Discuss management with haematologist and orthopaedic surgeon
- surgical drainage or sequestrectomy may be required
Other infections
- Infection is a major cause of morbidity and mortality in SCD
- Therapy of specific infections varies with the clinical setting
- see relevant guideline for suspected source of infection
BLOOD TRANSFUSION
General principles
- All patients should carry a transfusion card with details:
- ABO group, extended red cell phenotype, Rh phenotype and
- existence of any red cell alloantibodies (current and historic)
- Transfusion history is important, particularly if care is in a different hospital
- liase with transfusion laboratory at primary hospital to get transfusion history
- Advise transfusion laboratory/blood bank that transfusion is for a patient with SCD
- Discuss with haematology to determine if simple top-up or exchange transfusion needed
- Determine post-transfusion target Hb and HbSS
- Record and document transfusion triggers and indications
- Monitor closely both during and after completion of transfusion for
- immune haemolytic transfusion reaction (IHTR)
- delayed haemolytic transfusion reaction (DHTR) and
- hyper haemolysis
- All patients should have annual viral screening for Hepatitis B, C and HIV 1 and 2
Venous access
- Simple top-up transfusion: single peripheral venous cannula
- Manual exchange transfusion: 2 separate large bore venous access
- one for transfusion and inlet port (wide bore needle grey/orange) and
- another for venesection (vascath: femoral/central neck line)
- Automated red cell exchange: femoral line/vascath – double lumen
- Long-term transfusion programme: consider a port-a-cath
Top-up transfusion
Indications
- Severe anaemia (Hb <50 g/L) owing to:
- hepatic or splenic sequestration
- red cell aplasia or haemolysis
- Severe anaemia when decrease in Hb >20% from baseline in a symptomatic patient (heart failure, dyspnoea, hypotension and marked fatigue)
- Transfuse to baseline Hb (patient’s Hb in steady state)
- Consider when exchange transfusion indicated and starting Hb <50 g/L.
- Discuss with haematologist
Exchange transfusion
Indications
- Severe chest syndrome
- New ischaemic stroke
- Multi-organ failure
- Consider in priapism
- Do not initiate exchange transfusion before discussing with haematologist
Targets
- To reduce HbS to <30%
- To maintain Hb <100 g/L
- note: haematocrit of donor blood is approximately double that of patient
- To maintain steady blood volume throughout procedure
Venous access
- Ideally, identify 2 ports for venous access; 1 for venesection, the other for transfusion
- in emergency, consider a central line, or arterial line (e.g. on ITU)
- Perform exchange transfusion isovolaemically (equal quantities in and out)
- Ensure patient well hydrated before exchange
- prehydrate with sodium chloride 0.9% 500 mL as first 500 mL of blood is being removed
- then give sodium chloride 0.9% 500 mL concurrently
- do not remove blood until venous access for transfusion is secure
- continue to administer IV fluids between transfusions at standard rate of 3 L/m2/24 hr
- See Blood and blood products guidelines
Method
- Usually requires at least 2 exchanges, each of 4 units venesected and 4 units transfused
- Venesect 500 mL of blood and simultaneously infuse 500 mL sodium chloride 0.9% at same speed as the bleeding
- As second 500 mL (and subsequent units) venesected, transfuse first unit of blood over 1–2 hr
- Venesect 500 mL and replace with blood and sodium chloride 0.9% five more times
- discuss in advance with haematologist
- Check interim Hct and Hb
- A simple top-up transfusion may be required following isovolaemic exchange transfusion
- Post-RBC exchange – FBC and Hct
DISCHARGE AND FOLLOW-UP
- Discharge home when pain controlled by oral medication
- Provide 3–4 days’ supply of analgesia
- Do not prescribe parenteral opioids TTO
- Provide patient or carer with information on the continuing management of the current episode including how to:
- obtain specialist support
- additional medication
- manage any potential side effects of treatment
© 2022 The Bedside Clinical Guidelines Partnership.
Created by University Hospital North Midlands and Keele University School of Computing and Mathematics.
Research and development team: James Mitchell, Ed de Quincey, Charles Pantin, Naveed Mustfa