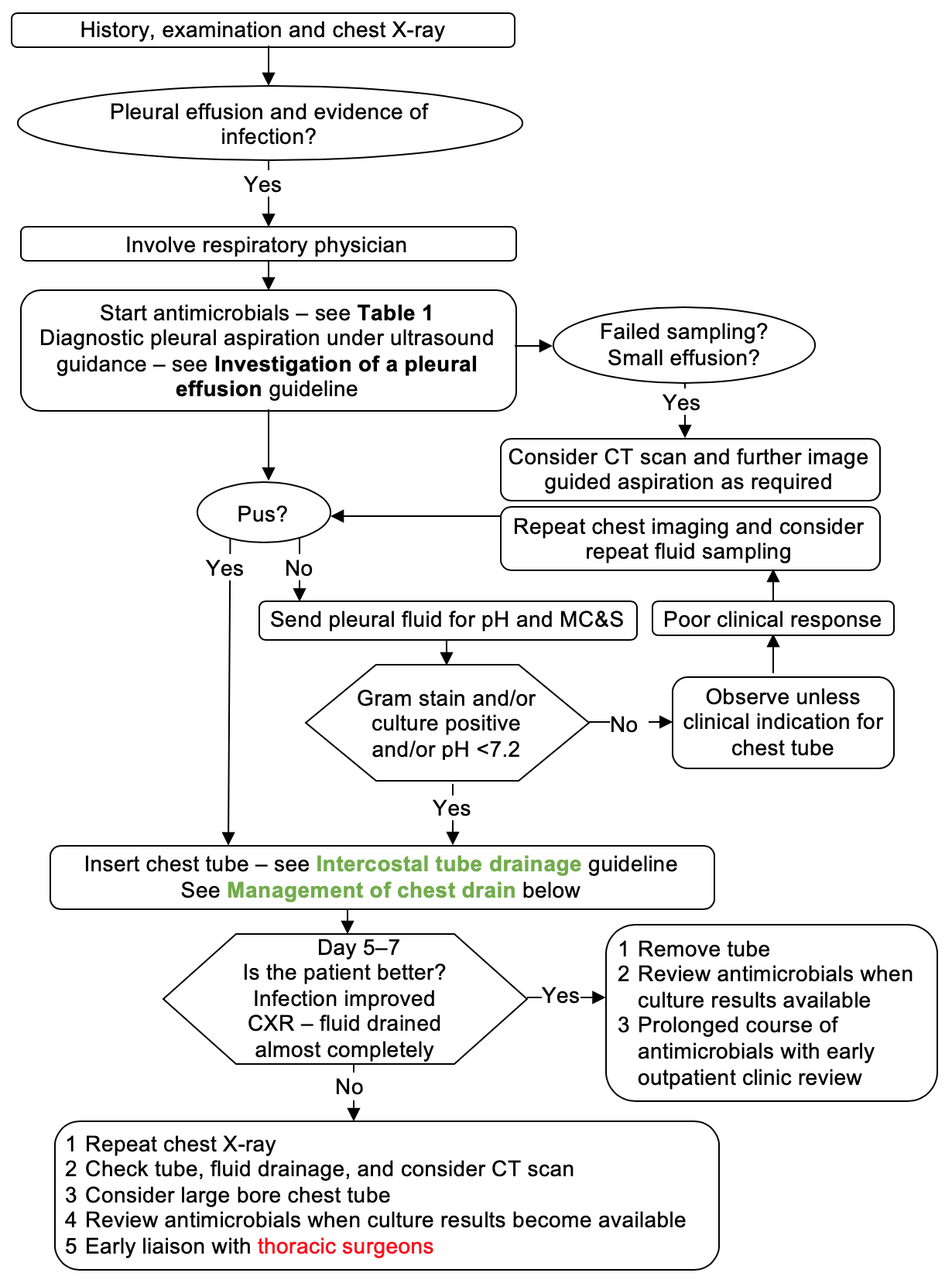
RECOGNITION AND ASSESSMENT
- Take history, clinical examination and chest X-ray
- If a pleural effusion with no evidence of infection, see Investigation of a pleural effusion guideline
INITIAL MANAGEMENT
- Involve respiratory physician
- Diagnostic pleural aspiration under ultrasound guidance
- Treatment is both drainage of the infected pleural fluid and antimicrobials
Appearance of aspirated fluid
- Send samples for M, C&S
- Insert chest tube – see Intercostal tube drainage guideline
- Send samples for: cytology, protein, LDH, glucose, pH, Gram stain, culture and sensitivity and TB cultures
- take blood at same time for LDH, protein and glucose
- If chylothorax suspected, send samples for cholesterol and triglyceride and for centrifuging
- If haemothorax suspected, send sample for haematocrit
- If rheumatoid disease suspected, send samples for glucose and complement
- If pancreatitis suspected, send sample for amylase
- Consider CT scan and further image-guided aspiration
Result of pleural fluid microscopy
Infection
- Insert chest tube – see Intercostal tube drainage guideline
Pleural fluid aspiration non-diagnostic
- Check if other diagnosis. See Investigation of a pleural effusion guideline
- Unless clinical indication for chest tube, observe
- If poor clinical response, repeat chest imaging and consider repeat fluid sampling
Antimicrobial therapy
- Unless absolutely impossible, send sample of fluid for culture before starting antimicrobial therapy
- If microbe known, follow advice of microbiologist / ID consultant
- Otherwise start empirical therapy while awaiting results of culture
Infection Control alerts
- Check for IC alert
- if IC alert not available, check previous 12 months of microbiology reports
- If MRSA present, treat as tagged for MRSA. See MRSA management
- if ESBL, MGNB, CARB present, treat as tagged for ESBL. See ESBL/MGNB/CARB management
Penicillin Allergy
- True penicillin allergy is rare
- Ask the patient and record what happened when they were given penicillin
- If any doubt about whether patient is truly allergic to penicillin, seek advice from a microbiologist or consultant in infectious diseases
Accept penicillin allergy as genuine hypersensitivity only if history of either rash within 72 hr of dose or anaphylactic reaction is convincing
Empirical antimicrobial regimen
- First line: Co-amoxiclav 1.2 g IV 8-hrly
- Alternative (true penicillin allergy): Levofloxacin 500 mg IV by infusion 12-hrly plus metronidazole 500 mg IV by infusion/or 400 mg oral 8-hrly
- if patient tagged for MRSA, add vancomycin IV by infusion (see Vancomycin guideline and calculator)
- if MRSA proven (cultured in pleural fluid) or likely cause of empyema (e.g. recent relevant specimen other than pleural fluid positive for MRSA): Discuss use of additional antimicrobial (e.g. rifampicin) with microbiologist/ID Consultant
SUBSEQUENT MANAGEMENT
- Nutritional support in prolonged illness
Management of chest drain
- Ensure chest tube is draining freely and the tube is swinging at all times.
- For small bore (12–18F) catheters, use the 3-way tap to flush with sodium chloride 0.9% 30 mL every 6 hr if not draining freely
- No flushing required for larger bore drains
Removal of tube
- When the patient better with:
- infection improved and
- CXR showing fluid drained almost completely
Oral antimicrobials
- Change to oral as soon as clinical improvement occurs and temperature normal for 24 hr
- providing there is no contra-indication to oral therapy and sensitivities allow
- Use oral antimicrobial to which microbe sensitive with good tissue penetration
- if not known or in doubt, discuss with microbiologist or consultant in infectious diseases
Duration of antimicrobials
- At least 3 weeks: continue antimicrobial therapy for a prolonged period of time
- usually at least until all fluid has gone and drain has been removed
- Monitor patient closely for recurrence after stopping treatment
Failure to respond to therapy
- Review by respiratory consultant/consultant in infectious diseases
- Repeat Chest X-ray
- Check tube, fluid drainage, and consider CT scan
- Consider large bore chest tube
- Review antimicrobials when culture results become available
- Early liaison with thoracic surgeons
DISCHARGE AND FOLLOW-UP
- Discharge when chest drains removed and clinical variables stable
- Continue antimicrobials for at least 3 weeks after initiation
- Follow all up patients in respiratory clinic with Chest X-ray about 3–4 weeks after discharge
© 2022 The Bedside Clinical Guidelines Partnership.
Created by University Hospital North Midlands and Keele University School of Computing and Mathematics.
Research and development team: James Mitchell, Ed de Quincey, Charles Pantin, Naveed Mustfa