INDICATIONS
- Infusion of drugs irritant to veins
- Long-term IV feeding, antimicrobials, chemotherapy (especially tunnelled catheters)
- Persistently difficult peripheral venous access
- Insertion of Swan-Ganz catheter or intracardiac pacing device
- Use of invasive cardiac output monitoring device that requires CVC
CONTRAINDICATIONS
- Sepsis at cannulation site
- Carotid artery aneurysm (precludes use of internal jugular vein on same side)
- Coagulopathy – hypo and hypercoagulation states
CONSIDERATIONS
Danger of serious morbidity
- If not competent in procedure, organise supervision by a clinician experienced in the procedure
Sterility is essential
- Perform technique in a sterile environment where possible
- e.g. treatment room, critical care or theatre suite
- Perform procedure using full sterile technique
- Use correct equipment
- Ongoing attention to sterility of line and dressings by all users
- Removal of line when no longer required
Use of ultrasound
- Equipment and assistance to place line under 2D imaging ultrasound guidance is present in theatres and critical care
Internal jugular vein
- If in elective situation, use 2-dimensional (2D) imaging ultrasound guidance
Subclavian vein
- Consider dynamic (real-time) 2D ultrasound for subclavian vein CVC insertion
- fewer complications and a higher success rate than landmark techniques
- 2D imaging ultrasound should be available in areas where central line cannulation is carried out on a regular basis
EQUIPMENT
- Sterile gloves, hat, mask, gown and full sterile drapes
- Dressing pack with gauze swabs, gallipots
- Scalpel holder with blade size 11
- Skin antiseptic. If not allergic to alcoholic chlorhexidine gluconate use 2% solution
- if allergic (but not to iodine) use alcoholic povidone-iodine solution
- Lidocaine 1% plain in a 5 mL syringe fitted with an orange (25 G) needle
- Sodium chloride 0.9% in a 20 mL syringe
- For catheters which require heparin lock, heparinised saline 10 units/mL in a 5 mL syringe
- 0 or 1 silk or nylon suture
- For peripherally inserted catheters, tourniquet
- Pressure transducer set
- Sodium chloride 0.9% (500 mL bag)
- Bionector® (Vygon) hubs for three-way taps
- prevent repeated unscrewing of ports for access to line
- if cleaned with each use, reduce infection
- Sterile clear semi-permeable occlusive dressing, or antimicrobial CVC dressing
CATHETER AND SITE
- Compare risk of infection against risk of mechanical complications
Patient-specific risks
- Pre-existing catheters
- Anatomical deformity
- Bleeding diathesis
- Some types of positive pressure ventilation
Relative risk of mechanical complications
- Bleeding
- Thrombosis
- Pneumothorax
Risk of infection
- To reduce risk of infection, consider peripherally inserted (arm) catheter
Arm vein
- Infection risk low
- Minimum length of catheter is 600mm
External jugular vein
- Infection risk medium
- Minimum length of catheter is 200mm
Subclavian vein
- Infection risk medium
- Minimum length of catheter is 150mm
Internal jugular vein
- Infection risk high
- Minimum length of catheter is 150mm
Catheter type
Long-term use
- For patients in whom long-term (>3–4 weeks) vascular access is likely, use tunnelled catheter or implantable vascular access device
Lumens
- Unless multiple ports are essential for patient management, use single-lumen catheter
Total parenteral nutrition
- Use single-lumen catheter or designate one port exclusively for this purpose
High risk of catheter-related bloodstream infection
- For adult inpatients who require short-term (1–3 weeks) central venous catheterisation, use antimicrobial impregnated central venous access device (CVAD)
- if all other aseptic precautions are instituted, further reduces infection
Chlorhexidine allergy
- do not use chlorhexidine impregnated cannula
PROCEDURE
Consent
- Explain procedure and reassure patient
- check patient not allergic to skin antiseptic
- Obtain and record consent
Position of patient and site of insertion
- Place patient into correct position for chosen approach
- Check site of introduction
Aseptic technique
- Scrub up using full sterile technique
- don gown, gloves, hat, mask and face and eye protection
- Prepare skin with antiseptic
- Drape operative field
Local anaesthetic
- Attempt aspiration on syringe before injection to ensure needle is not intravascular
- Local anaesthetic may not be necessary in anaesthetised patients
INSERTION OF CVC
- Check fit and function of equipment
Maintain venous pressure above atmospheric
- Whichever vein used, maintain venous pressure above atmospheric by correct position or tourniquet on limb to avoid air embolism
Antecubital fossa – median (basilic) or cephalic veins
- Place patient in what position?
- Distend veins by tourniquet
- Turn head to same side to compress neck veins
- Abduct arm
- Partially insert catheter then release tourniquet
- before releasing tourniquet, position proximal end of catheter below level of patient's elbow to avoid air embolus
- advance catheter to predetermined length
- Catheter passage through cephalic vein may be impeded by fascia deep to axillary vein
External jugular vein
- Place patient at 20° head down
- Vein runs from angle of mandible to behind middle of clavicle
- Choose most prominent of the right or left veins
- STOP if no vein visible or palpable
- Turn patient's head to contralateral side
- Insert catheter >200 mm length
- In 50% of patients, catheter cannot be threaded into an intrathoracic vein
- if so, try finger pressure above clavicle, depressing shoulder, or flushing catheter
- use of Seldinger or a spiral J-shaped wire may help
- DO NOT use excessive force
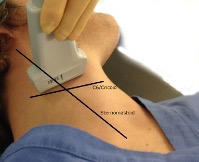
Internal jugular vein
- See Figure 1
- Place patient at 20° head down with head turned to contralateral side
- Preferentially use right jugular vein running behind sternomastoid close to lateral border of carotid artery
- not left to avoid injury to thoracic duct
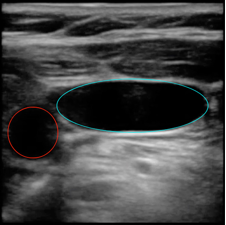
- Use 2-D imaging ultrasound guidance to identify vein and correct placement of guidewire
- see Figure 2
- Insert cannula
- operators of limited experience can try cannulation with the smaller locator needle/catheter to locate vein first and then use that as guide
- if artery is punctured, compress firmly for ≥5 min
AFTER INSERTION
- Aspirate blood on all lumens to check catheter position before injecting fluid
- On connection to pressure transducer, CVP waveform should be visible, not arterial
- Fix catheter with suture at clip site and securing holes at hub for internal jugular lines
- Cover insertion site with a clear sterile dressing
Chest X-ray
- Look for pneumothorax
- Check tip of a right-sided line is at or above the level of the carina
- confirms tip of catheter lies above pericardial reflection to avoid arrhythmias and perforation
- A left-sided line should ideally lie above the carina but:
- preferable to have the line in the SVC lying parallel to the vein (e.g. in a vertical position) rather than abutting against the wall of the SVC or lying high in the innominate vein
COMPLICATIONS
Injury to vital structure
- Pneumo- or haemothorax, arterial puncture
- Damage to thoracic duct or phrenic nerve
Arterial insertion
- Confirm by placing a small gauge cannula over guide wire and into vessel and transducing pressure before dilation
Tear of vein
- Avoid by inserting dilator no more than a few cm
Kinking of guide wire
- Avoid a perpendicular approach into vein
Air or guidewire embolus
- Place patient in head-down position during insertion of line
- If not in use ensure all ports closed and clamped
- Do not lose sight of guidewire externally at any time
Cardiac arrhythmias
- Usually stop spontaneously
- If persistent, withdraw catheter into SVC
- If severe, treat
Perforation of myocardium, mediastinum or pericardium
- Ensure free aspiration of each lumen
- Transduce main lumen and check position on X-ray
- If suspected, withdraw catheter and stop infusion
Infection, local or systemic sepsis
- Take great care with aseptic technique
AFTERCARE
Strict asepsis at all times
- Change IV giving set as per hospital protocols using aseptic technique
- Use needleless connectors where available
- if possible, do not inject drugs or take blood samples through rubber bungs
- Maintain continuous flow through catheter to prevent clotting
- if clotting occurs, try to clear by injecting 2–5 mL heparinised sodium chloride 0.9% 10 units/mL under pressure
Infection
- Monitor venepuncture site for infection daily
- If an infection occurs, see Management of central catheter-related sepsis in Artificial nutritional support in Surgical guidelines
© 2022 The Bedside Clinical Guidelines Partnership.
Created by University Hospital North Midlands and Keele University School of Computing and Mathematics.
Research and development team: James Mitchell, Ed de Quincey, Charles Pantin, Naveed Mustfa