RECOGNITION AND ASSESSMENT
- Parkinson’s Disease (PD) is characterised by:
- tremors, rigidity, akinesia, postural instability
- decline in swallowing function
- neuroleptic malignant syndrome
- range of non-motor complications (e.g. psychiatric and sleep disorders)
History
- Take an accurate drug history
- know precisely how PD is managed by patient
- taking their normal doses in recent days (e.g. too unwell to take as normal)?
- Consider all sources of information including:
- patient, usually well informed on their precise treatment
- summary Care Records/GP fax/GP phone call/previous TTO
- carer(s)/next of kin
- transferring hospital/nursing home/residential home prescription charts
- patient’s own drugs (PODs)/repeat prescriptions
- Computer letters and notes
INITIAL MANAGEMENT
- If possible, continue patient’s individualised PD treatment
- Discuss with a PD specialist whether dose adjustments may be required
- Prescribe all PD medications, specifying exact timings as necessary
- e.g. co-beneldopa 12.5/50 mg 6-hrly; 0600, 1000, 1400, 1800
- ensure supply of required PD medications are available
- Do not stop or miss doses of levodopa or dopamine agonists
- prescribe COMT inhibitors (e.g. entacapone) at the same time as levodopa-containing medicines
- Avoid medicines which may worsen PD
- antipsychotics (haloperidol). If necessary, consider a benzodiazepine
- anti-emetics (metoclopramide and prochlorperazine). If necessary, consider domperidone (if nausea not transient, think ECG QTc prolongation)
Apomorphine
- If already using apomorphine, continue current regimen
- Do not initiate apomorphine without involvement from a PD specialist
- APO-go (apomorphine) 24 hr helpline
Nil-by-mouth or compromised swallow
- Refer for urgent swallowing assessment
- Consider placing tablets on a teaspoon with thickened fluids/soft foods (e.g. yoghurt), or dispersible/liquid preparations
- Check for underlying cause and treat accordingly
- COMT inhibitors and MAOB inhibitors can be safely omitted temporarily
- If already using apomorphine injection or infusion, continue current regimen
- do not initiate apomorphine without involvement from a PD specialist
Patient not able to take next oral dose
- Priority: maintenance of dopaminergic medication
- Refer patient to PD specialist and swallowing team ASAP. If unable to contact (e.g. out-of-hours):
- if NG tube placement possible, give via enteral feeding tube at usual times. For advice on doses via enteral feeding
- if NG tube placement impossible, convert to equivalent dose of rotigotine patch. For advice on dose of rotigotine patch
Rotigotine patch administration
- Apply patches once a day. Press firmly on back of patch for a minimum of 30 seconds onto skin to activate adhesive – see Figure 1
- Apply patch at approximately the same time each day
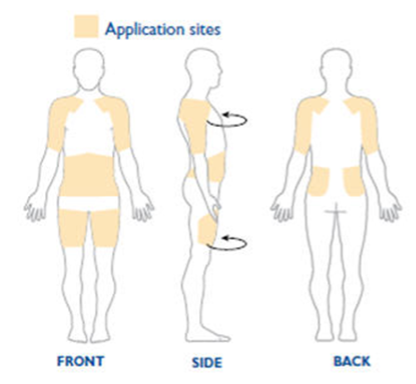
- Rotate application site daily to reduce risk of skin irritation (do not use same area of skin again for 14 days). See Figure 2 for suggested application sites
Monitor patient
- 4-hrly observations including
- sedation
- respiratory rate
- application site
- response
- If increased stiffness/slowness, increase dose and review daily
- If increased confusion/hallucinations, decreased
SUBSEQUENT MANAGEMENT
- Decided by PD specialist