PAIN
- Pain is common in patients with life-limiting illness
- Physical, psychological, social and spiritual factors can influence the experience of pain
- Pain can be well controlled in the majority of patients
Types of pain
- Visceral/soft tissue pain
- likely to be opioid sensitive
- Bone pain
- often partially opioid sensitive
- may respond to NSAIDs, radiotherapy and bisphosphonates
- Nerve pain
- partially opioid sensitive
- may respond well to adjuvant analgesics
Pain assessment
- Take a pain history using SOCRATES
- S – Site
- O – Onset
- C – Character
- R – Radiation
- A – Associated symptoms
- T – Timing
- E – Exacerbating and relieving factors
- S – Severity
- Use a pain scale
- 0–10
- visual analogue scale
- Analgesic history
- current analgesia
- previously tried analgesia
- effectiveness of treatment
- side effects of treatment
PAIN MANAGEMENT
Principles
- Identify and treat cause of pain if possible
- Select treatment appropriate for the pain and patient’s needs
- Keep it simple and use oral medication whenever possible
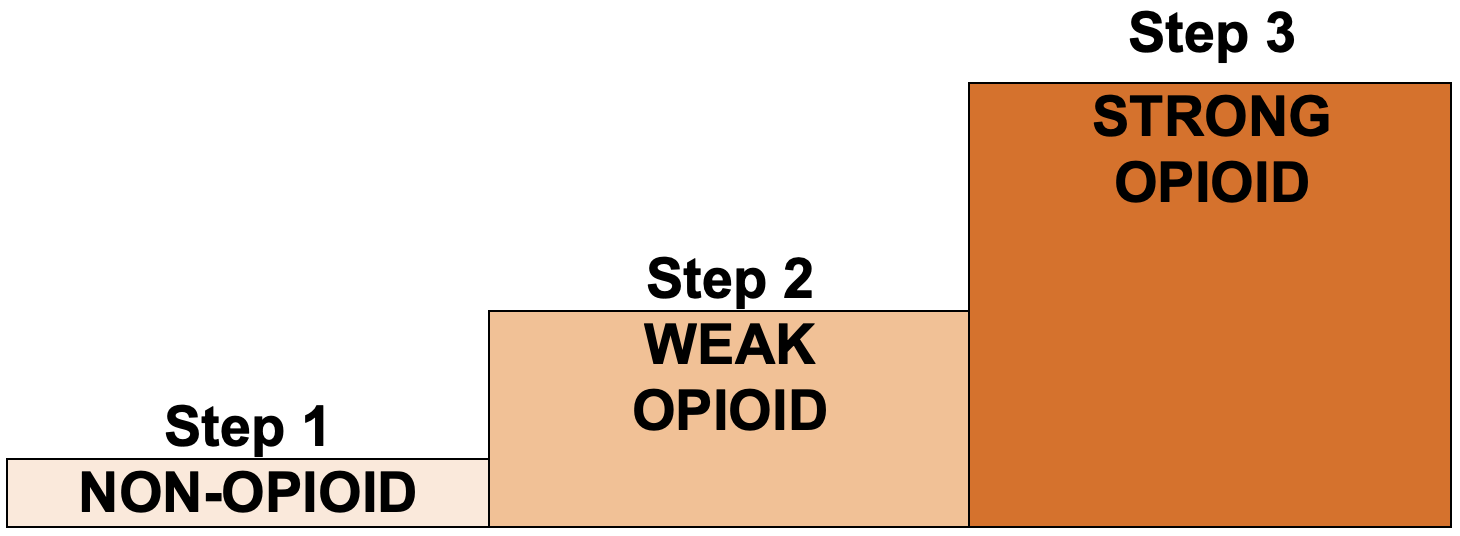
- Pain relief should be by the mouth (oral), by the clock (regular) and by the WHO analgesic ladder
- add adjuvant analgesics (e.g. NSAID/anticonvulsant/antidepressant/antispasmodic) with any step
Step 1 – non-opioid
Paracetamol
- Analgesic and antipyretic
- Dose: 500 mg–1 g 4–6 hrly (maximum dose 4 g in 24 hr)
Non-steroidal anti-inflammatories – NSAIDs
- Anti-inflammatory, anti-pyretic and analgesic
- 1st line NSAID – ibuprofen
- 1.2–2.4 g daily in 3–4 divided doses
Caution
- See BNF for cautions and contraindications before starting NSAID
- History of gastroduodenal ulceration – prescribe gastroprotective drug (e.g. PPI)
- Concomitant corticosteroids or anticoagulant – prescribe gastroprotective drug (e.g. PPI)
Step 2 – weak opioid
- Useful for moderate pain
- Seldom useful to change from one preparation to another
- If regular doses do not provide adequate analgesia, move up WHO analgesic ladder to Step 3
- Prescribe regular laxative to prevent constipation
Drugs
- Codeine 30–60 mg 4-hrly (maximum dose 240 mg in 24 hr)
- Co-codamol available as:
- 8/500 (codeine 8 mg with paracetamol 500 mg)
- 30/500 (codeine 30 mg with paracetamol 500 mg)
- dose: 2 tablets 4–6 hrly (maximum 8 in 24 hr)
Step 3 – strong opioid
- If regular weak opioid not controlling pain, initiate modified release morphine (e.g. Zomorph®, MST®)
- usual starting dose 10–15 mg oral 12-hrly
- remember 60 mg codeine 6-hrly is equivalent to 24 mg oral morphine in 24 hr
- Also prescribe as required immediate release morphine (e.g. morphine sulphate solution) for breakthrough pain
- prescribe one-sixth of the total daily dose of regular morphine (usually 2.5–5 mg)
Communication
- Ask about and discuss any concerns and misconceptions about starting strong opioids
- Provide verbal and written information on the use of strong opioids
- how to take them
- side effects
- safe storage
- how pain will be reviewed and who to contact if any problems
- If patient wishes to continue to drive, give verbal and written advice on the law on driving when taking opioid medications
Review and titration
- Nursing assessment of pain at least 4-hrly (e.g. drug rounds, observations)
- Medical review of pain control 24–48 hr after starting regular strong opioids
Patient still experiencing pain and pain is opioid sensitive
- Consider increasing regular dose
- add up total amount of morphine given in last 24 hr including modified release and immediate release morphine. Divide by 2 and prescribe 12-hrly (rounded to the nearest 5 mg)
- ensure dose of as-required immediate release morphine is adjusted when the dose of modified release morphine changed. It should be one sixth of the total daily dose of regular morphine
- see Example
Side effects
- Constipation can occur with all opioids
- prescribe regular laxatives when prescribing regular strong opioids
- it may be necessary to increase the dose of laxatives as the dose of morphine increases
- Nausea may occur when strong opioids started or dose increased but this is likely to be transient
- if nausea develops, use regular haloperidol 1.5 mg oral or SC at night
- consider stopping after 5 days
- Drowsiness or impaired concentration may occur when strong opioids started or at dose increase. If persistent or severe:
- if pain controlled, reduce dose
- if pain not controlled, consider switching to alternative opioid. See Alternative opioids below
- if side effects persist or considering alternative opioids, refer to hospital palliative care team
Alternative opioids
- May be used to improve side effect profile
- Oxycodone is the preferred second line opioid
- Do not use fentanyl patches to manage uncontrolled pain due to long half-life
- See Opioid equivalence tables
- use dose in equivalence table as an approximate guide
- If considering alternative opioid preparations, seek advice from hospital palliative care team
Opioids by continuous subcutaneous infusion
- Unless there is a problem with absorption or administration, opioids via continuous subcutaneous infusion will not provide better analgesia than oral route
- See Continuous subcutaneous infusion (CSCI) in palliative care guideline
© 2022 The Bedside Clinical Guidelines Partnership.
Created by University Hospital North Midlands and Keele University School of Computing and Mathematics.
Research and development team: James Mitchell, Ed de Quincey, Charles Pantin, Naveed Mustfa