INDICATIONS
Diagnosis
- Aspirate an acute hot joint of uncertain origin before starting any antimicrobials
- Often used in diagnosis of chronic and subacute articular pathologies
Treatment
- Recurrent aspiration in management of septic arthritis
- Aspiration of tense effusions of any cause
- Before therapeutic intra-articular corticosteroid injection
CONTRAINDICATIONS
- No absolute contraindications to joint aspiration
- Caution in patient with clotting disorder/taking anticoagulants. Discuss with consultant
- Caution in patient with prosthetic joint. Discuss with orthopaedic surgeon
- Avoid passing needle into joint through skin lesion (e.g. psoriasis), as this can lead to joint sepsis
EQUIPMENT
- Sterile dressing pack
- Gloves
- Skin antiseptic
- 20, 10 and 2 mL syringes, green and orange needles
- Lidocaine 1% plain
SPECIMEN BOTTLES
- Blood culture bottles for aerobic and anaerobic culture of synovial fluid
- 2 plain sterile universal containers:
- 1 for Gram staining
- 1 for crystals
- Heparin tube – for white cell count (orange top)
PROCEDURE
- If not competent in procedure, organise supervision by a clinician experienced in the procedure
Consent
- Explain procedure and reassure patient
- Obtain and record consent
Position of patient and site of insertion
- Ask patient to lie supine
- Make sure muscles around joint are relaxed to minimise any discomfort from procedure
- putting pillow under knee may help to relax it
- Identify margins of knee joint and patella
- Mark a point (e.g. with thumbnail) 1 cm below mid-point of medial aspect of patella
Aseptic technique and premedication
- Wash your hands, don gloves, prepare skin around knee
- Infiltrate skin with lidocaine 1% using an orange needle
Sampling
- Use no-touch technique
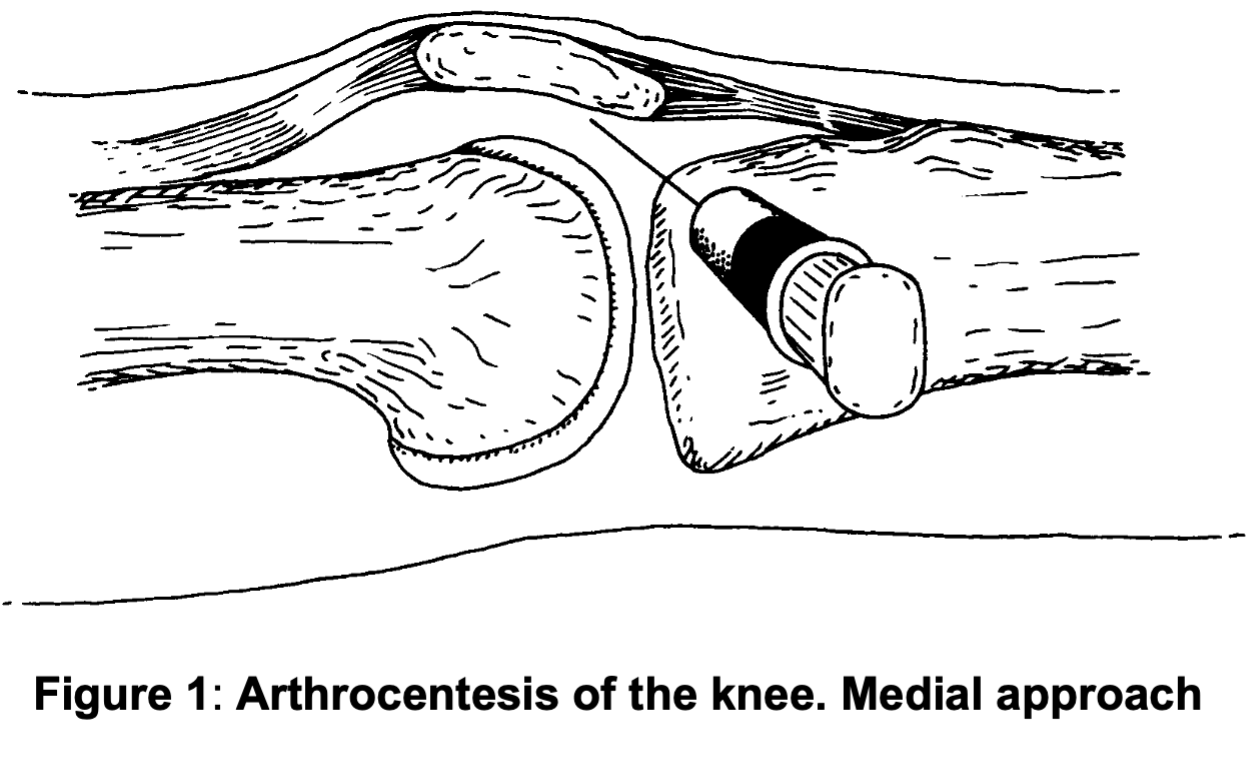
- Insert green needle with 10 or 20 mL syringe horizontally at previously marked point into gap between patella and femur and slightly upward towards suprapatellar pouch
- see Figure 1
- if there is only a small effusion, it can help to displace patella medially to increase gap between patella and femur (Figure 1)
- Aspirate while advancing needle and stop advancing if synovial fluid aspirated
- once fluid begins to appear, it can be ‘milked down’ by pressure with one hand over suprapatellar pouch
- Once syringe full, detach from needle, leaving needle in joint
- Empty syringe into specimen bottles
- 8–10 mL of fluid directly into aerobic bottle first, followed 8–10 mL into anaerobic bottle, rest into plain sterile universal container
- Re-attach syringe to needle and re-aspirate
- Aspirate joint to dryness
- When aspiration complete, withdraw needle
- An adhesive plaster or Micropore dressing to skin is sufficient
Documentation
- Record procedure in notes
- Document exact joint aspirated with:
- volume of fluid
- macroscopic appearance (‘frank pus’, ‘turbid straw-coloured fluid’, ‘frank blood’, ‘blood-stained synovial fluid’, etc.)
- viscosity (‘viscous’ or ‘thin’) of fluid
SPECIMENS
- Send synovial fluid in blood culture bottle and one plain sterile universal container to microbiology
- request urgent Gram stain
© 2022 The Bedside Clinical Guidelines Partnership.
Created by University Hospital North Midlands and Keele University School of Computing and Mathematics.
Research and development team: James Mitchell, Ed de Quincey, Charles Pantin, Naveed Mustfa