RECOGNITION AND ASSESSMENT
Symptoms and signs
- Nausea
- Cramps
- Confusion, seizures, varied CNS manifestations
- Unless serum sodium (Na+) falling rapidly, concentrations in range 125–135 mmol/L are usually asymptomatic
- Those of underlying cause
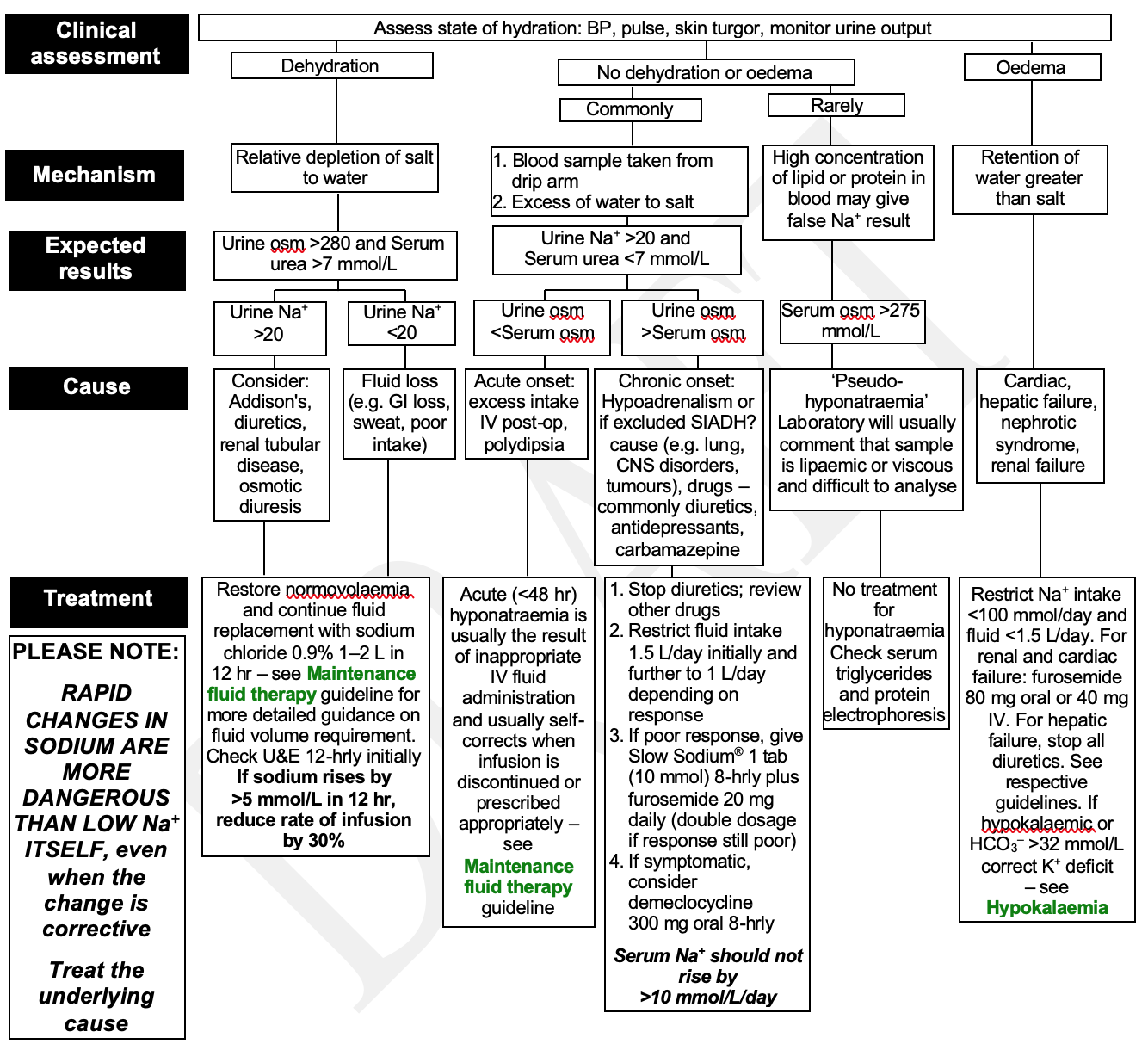
Clinical assessment
- Assess state of hydration: BP, pulse, skin turgor, monitor urine output
Investigations
- Take sample from arm without a drip
- FBC and U&E (eosinophilia, hyperkalaemia, or hypercalcaemia suggest hypoadrenalism)
- Glucose
- Osmolality (urine plus serum), urine Na+, TFT
MANAGEMENT
- Treat the underlying cause. For guidance follow Flowchart. Further information available from clinical biochemistry or from renal or endocrine teams
Sodium levels
- Monitor at least daily
- If a patient has a high urine output and/or very low Na <115 mmol/L, monitor electrolytes 4-hrly initially to avoid sudden rises in serum Na+
- Rapid changes in sodium are more dangerous than LOW Na+ ITSELF, even when the change is corrective
- Hypertonic saline is almost never justified, carries a significant risk, should be given only with consultant approval and requires monitoring in a high dependency area
- Failure to correct, or recurrence of hyponatraemia merits referral to the team appropriate to the underlying cause (e.g. renal, endocrine, psychiatric)
- Review drug treatment before discharge
Management flowchart tool