RECOGNITION AND ASSESSMENT
Symptoms and signs
- Often none, or neuromuscular symptoms (e.g. muscle weakness, absent reflexes, ileus)
Investigations
Immediate
- ECG changes – depressed ST, flat T, U waves, arrhythmias (arrhythmias may cause cardiorespiratory symptoms)
Helpful
- Repeat K+ (U&E). Take sample from arm without a drip
- Venous HCO3– – when raised (metabolic alkalosis) indicates chronic depletion; if <22 mmol/L in absence of GI loss, suspect renal tubular acidosis – refer to renal team
- Urine K+ if cause not obvious
- Serum magnesium (Mg2+) for persistent urine K+ loss especially patients with diarrhoea or on diuretics
Common Causes
- Blood taken from drip arm (artefact)
- Any excessive gastrointestinal fluid loss
- Renal loss: urine K+ >20 mmol/L – diuretics, mineralocorticoid excess (hyperaldosteronism and excess cortisol), Mg2+ deficiency see Hypomagnesaemia guideline, and renal tubular disease
- Intracellular shift (redistribution): insulin or bicarbonate treatment, theophylline, beta2 agonists, periodic paralysis, rapid blood cell proliferation
- Intravenous fluid therapy, with inadequate electrolyte replacement
MANAGEMENT
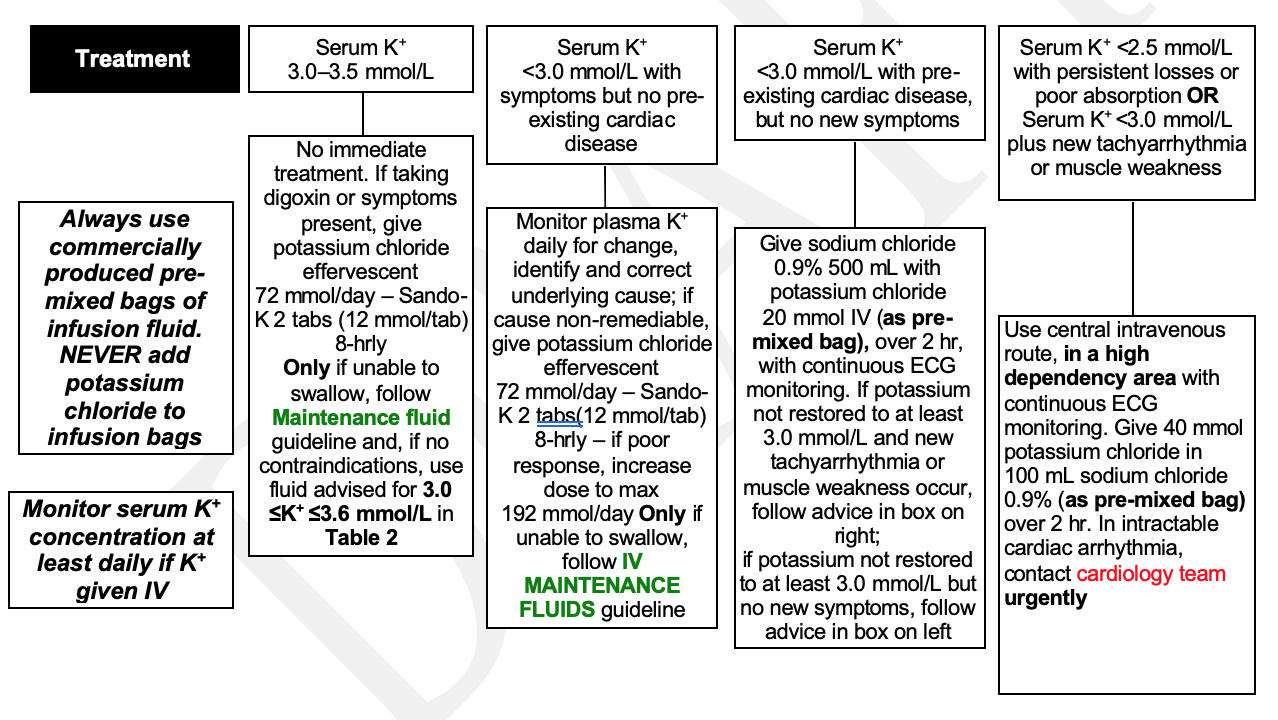
Always use commercially produced pre-mixed bags of infusion fluid. NEVER add potassium chloride to infusion bags
- Manage K+. For guidance follow flowchart
- If K+ given IV, monitor serum potassium concentration at least daily
- Treat the underlying cause. If cause not obvious, refer to renal or endocrine team for further evaluation
Management flowchart tool
© 2022 The Bedside Clinical Guidelines Partnership.
Created by University Hospital North Midlands and Keele University School of Computing and Mathematics.
Research and development team: James Mitchell, Ed de Quincey, Charles Pantin, Naveed Mustfa