In hyperkalaemia in a dialysis patient, contact renal team urgently for advice
In patients with DKA, follow Diabetic ketoacidosis guideline
In patients with DKA, follow Diabetic ketoacidosis guideline
RECOGNITION AND ASSESSMENT
- ABCDE approach and NEWS system
- Comprehensive medical and drug history and clinical examination to determine the cause of hyperkalaemia
Symptoms and signs
- Frequently none, or non-specific neuromuscular symptoms
- Muscular weakness may occur if blood K+ >7.0 mmol/L
- Cardiac arrest without warning
- ECG changes (see Treatment)
Investigations
- In emergency, measure K+ on a point-of-care blood gas analyser and initiate treatment whilst awaiting the results from a laboratory plasma sample (green top; lithium heparin)
- HCO3- in venous blood (or from blood gases, if indicated for other reasons) and lactate
- If serum K+ ≥6.0, urgent 12-lead ECG. If ECG abnormal, or rapid rise in K+ levels and in patients with plasma K+ ≥6.5 mmol/L, continuous 3 lead cardiac monitoring; ideally in a high-dependency setting
Common Causes
- Artefact: release from blood cells (e.g. during clotting, blood dyscrasias, haemolysis, delayed centrifugation of sample for >2 hr)
- Low molecular weight heparin
- Failure of excretion: renal failure, mineralocorticoid deficiency, drugs e.g. spironolactone, amiloride (potassium sparing diuretics), ACE inhibitors (~prils), angiotensin II blockers (~sartans), aliskiren, NSAIDs, ciclosporin, tacrolimus
- Release from cell: severe tissue damage, acidosis (consider DKA, lactic acidosis)
- Excess ingestion or supplementation
MANAGEMENT
- If refractory shock/other organ failure or cause not known, seek advice from ITU and or renal team
- Protect the heart and lower K+. For guidance follow algorithm (Management of Hyperkalaemia)
- Treat the underlying cause
Management of Hyperkalaemia
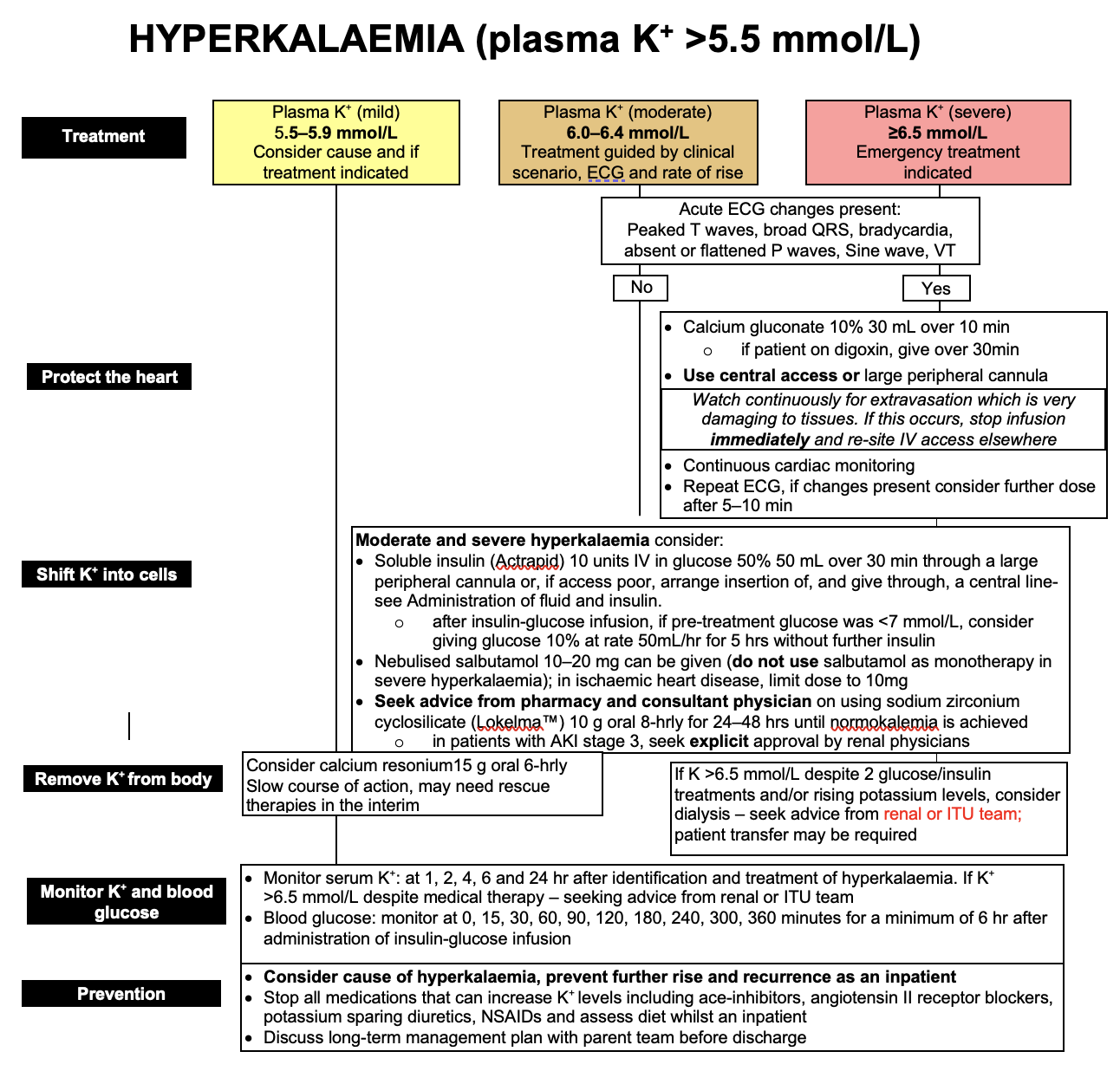
Prevention
- Consider cause of hyperkalaemia, prevent further rise and recurrence
- Stop all nephrotoxic medication including ace-inhibitors, angiotensin II receptor blockers, potassium sparing diuretics, NSAIDs and assess diet whilst an inpatient
- Discuss long-term management plan with parent team before discharge
Monitor
- Serum K+: at 1, 2, 4, 6 and 24 hr after identification of hyperkalaemia. If K+ >6.5 mmol/L despite medical therapy, seek advice from renal or ITU team
- Blood glucose: monitor at 0, 15, 30, 60, 90, 120, 180, 240, 300, 360 minutes for a minimum of 6 hr after administration of insulin-glucose infusion
© 2022 The Bedside Clinical Guidelines Partnership.
Created by University Hospital North Midlands and Keele University School of Computing and Mathematics.
Research and development team: James Mitchell, Ed de Quincey, Charles Pantin, Naveed Mustfa