ROUTINE BOWEL CARE
- Enquire about usual bowel habit
- If patient from nursing/residential home and unable to provide information, request the Home-to-Hospital form
- Enquire about laxatives from GP or bought over the counter
- Enquire about adverse effects from laxatives in the past
Risk factors
- Constipation likely in patients who are:
- immobile/less mobile than usual
- drinking less fluid than usual
- eating less cereal, fruit and vegetables than usual
- taking prescribed codeine and/or iron or post-operatively
- If taking opioids, prescribe laxatives routinely
Routine nursing care
- Complete bowels section on nursing sheets daily
- Encourage fluids (≥1 L/day)
- If patient usually takes prescribed laxatives, prescribe in hospital
Toileting
- Ensure toileting facilities provide safeguard privacy and dignity
- Transfer to toilet, if possible
- Avoid commode
- Prevent inhibition
- Ensure privacy
- Control noise (try to locate toilets in quieter part of ward)
- Ensure patient can easily summon help
- make bell or button accessible and respond promptly
- Control odours (use air freshener if necessary)
BOWELS NOT OPEN FOR 3 DAYS = CONSTIPATION
Cautions
- In patients with suspected intestinal obstruction, ask for senior advice
- take care when using laxatives of any kind
- If haemorrhoids or anal fissure, avoid rectal preparations
- In patients with inflammatory bowel disease, colitis or Crohn’s disease, avoid macrogols
Bowels not opened for >3 days
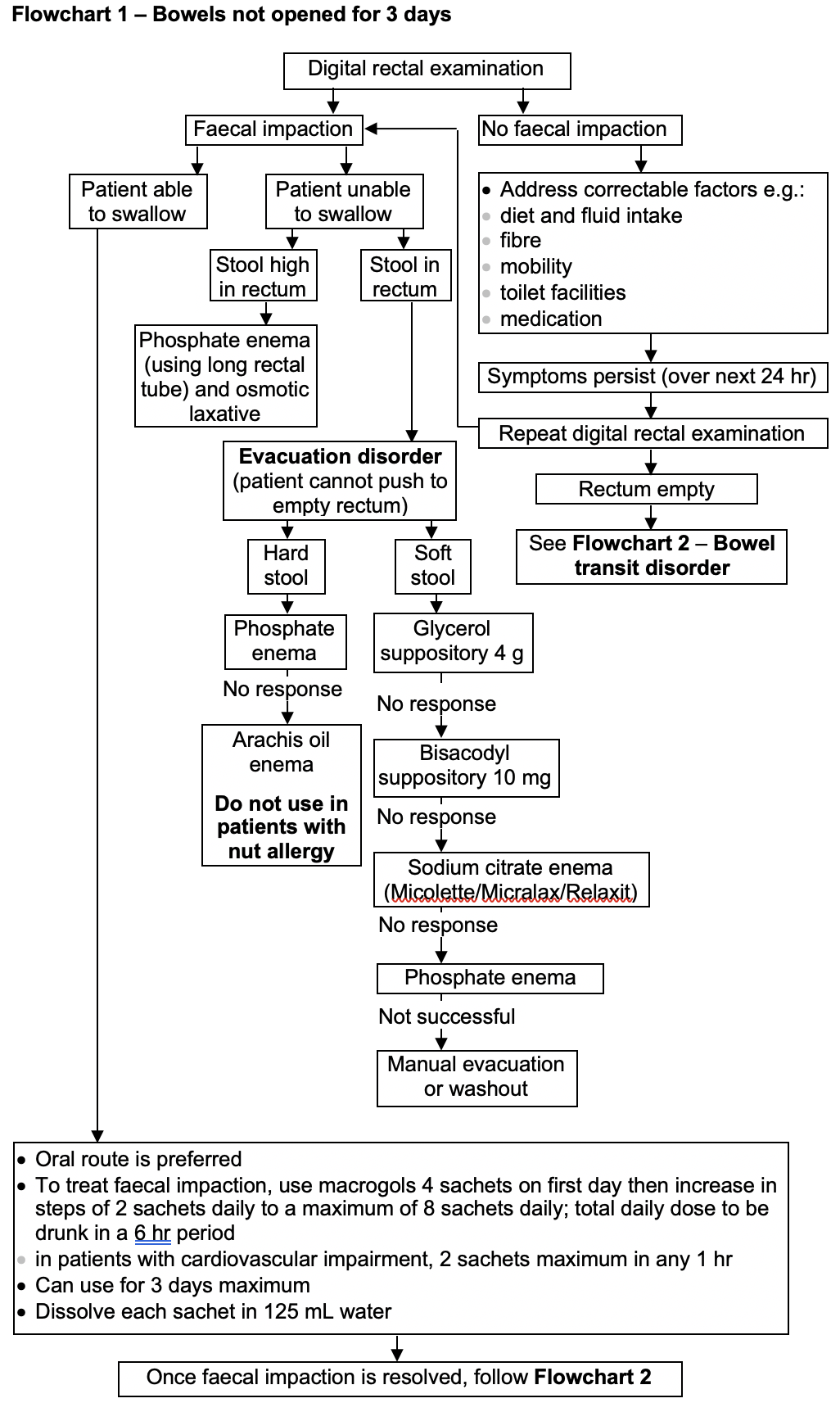
- Perform digital rectal examination
- document findings
- if rectum empty, follow No faecal impaction below
- if rectum full of faeces, follow Faecal impaction below
No faecal impaction
- Address correctable factors e.g.:
- diet and fluid intake
- fibre
- mobility
- toilet facilities
- medication
Symptoms persist (over next 24 hr)
- Repeat digital rectal examination
- document findings
- if rectum full of faeces, follow Faecal impaction below
- if rectum empty, follow Bowel transit disorder below
Faecal Impaction
Able to swallow
- Use oral route
- Macrogols 4 sachets on first day then
- increase in steps of 2 sachets daily
- maximum of 8 sachets daily
- Total daily dose to be drunk in a 6-hr period
- in patients with cardiovascular impairment, 2 sachets maximum in any 1 hr
- Dissolve each sachet in 125 mL water
- Use for 3 days maximum
- If faecal impaction is resolved, follow Bowel transit disorder below
- If faecal impaction is not resolved, discuss with consultant/SpR
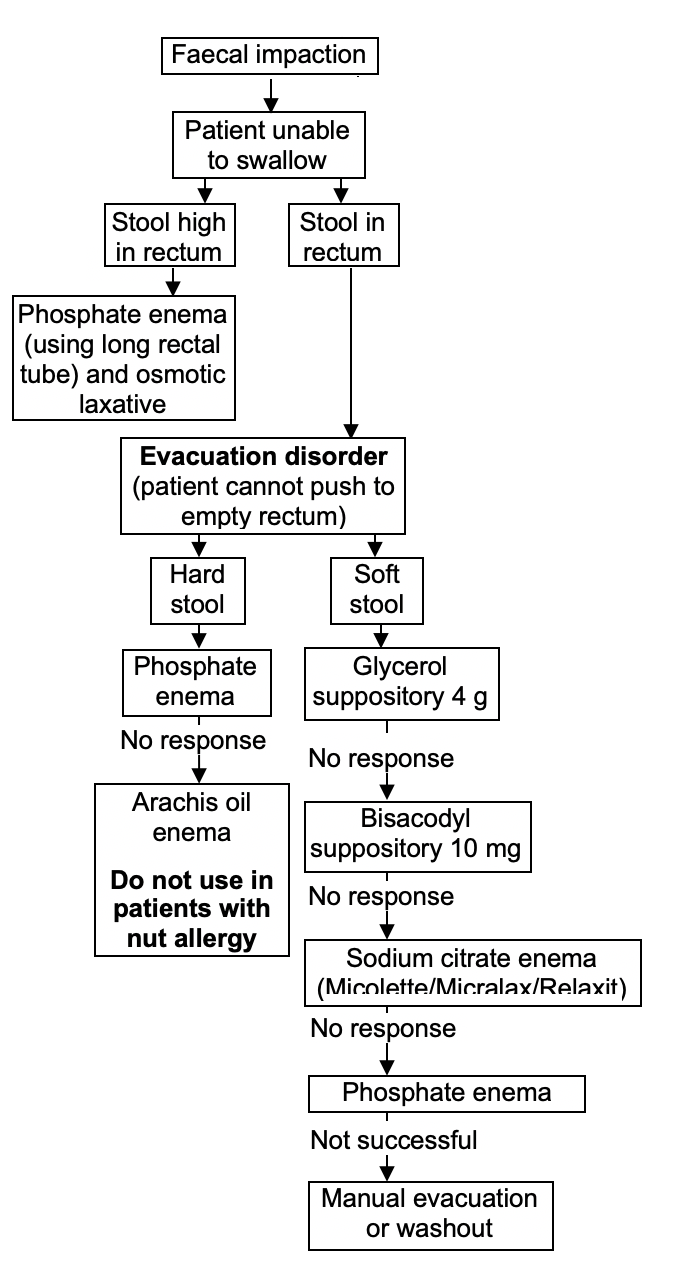
Unable to swallow
- Follow decision algorithm below
Decision algorithm (Unable to swallow)
Bowel transit disorder
- Patient constipated but rectum empty
- Follow decision algorithm below
Decision algorithm (Bowel transit disorder)
Select:
Not taking opioids nor has Parkinson’s disease/multiple sclerosis
- Macrogols 1–3 sachets in divided doses adjusted according to response
- Maximum duration of treatment 2 weeks
Response
- Symptoms relieved, no further treatment necessary
- Symptoms continue, consider Possible extra treatment for persistent symptoms below
Taking opioids or with Parkinson’s disease/multiple sclerosis
- Macrogols 1–3 sachets in divided doses adjusted according to response
Response
- Symptoms relieved, maintenance dose of macrogols 1–2 sachets daily indefinitely
- Symptoms continue (still constipated) after taking macrogols for at least 3 days, consider Possible extra treatment for persistent symptoms below
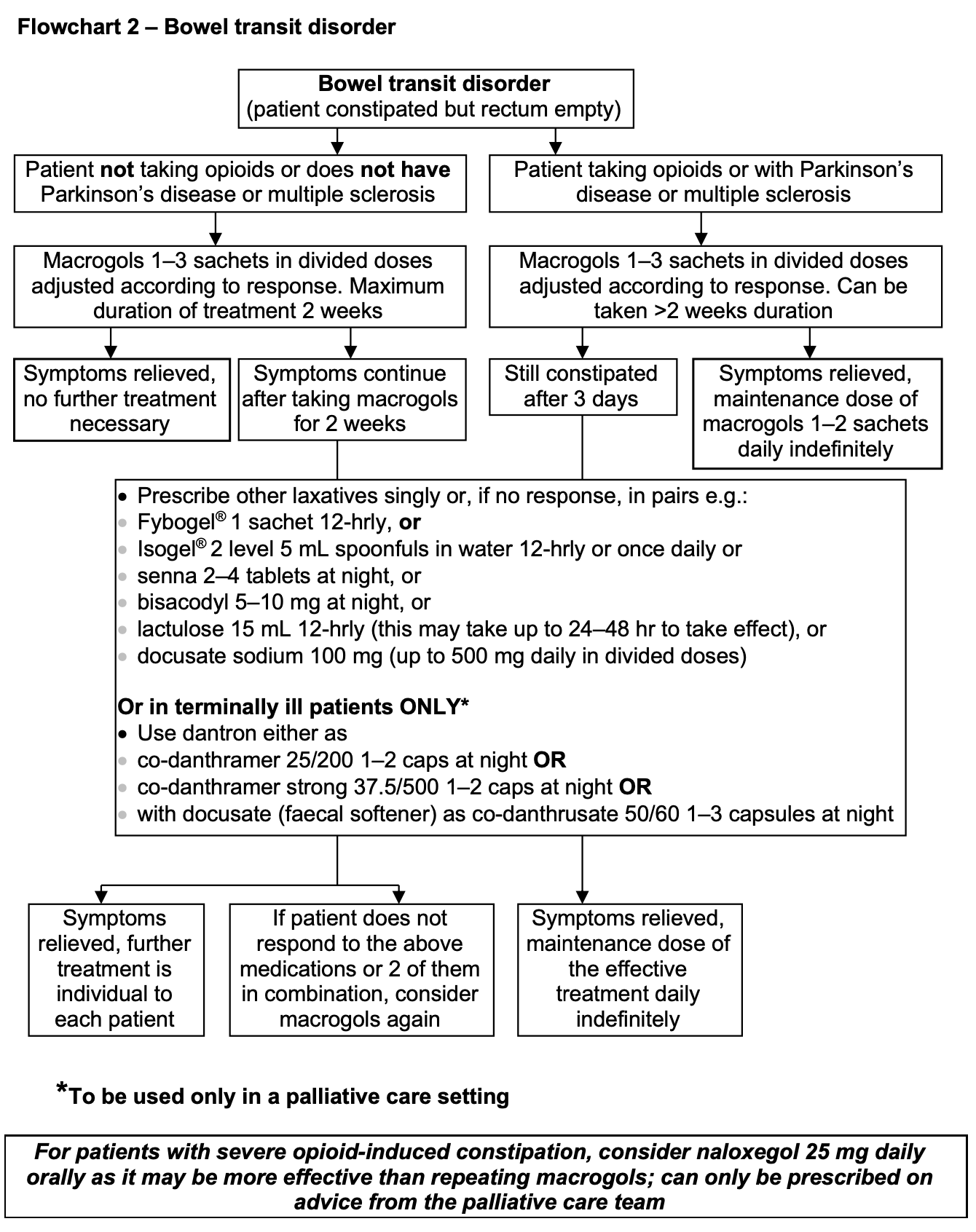
Possible extra treatment for persistent symptoms
- Prescribe other laxatives singly or, if no response, in pairs e.g.:
- Fybogel® 1 sachet 12-hrly, or
- Isogel® 2 level 5 mL spoonfuls in water 12-hrly or once daily, or
- senna 2–4 tablets at night, or
- bisacodyl 5–10 mg at night, or
- lactulose 15 mL 12-hrly (this may take up to 24–48 hr to take effect), or
- docusate sodium 100 mg (up to 500 mg daily in divided doses)
- In terminally ill patients in a palliative care setting ONLY, consider dantron
- co-danthramer 25/200 1–2 caps at night OR
- co-danthramer strong 37.5/500 1–2 caps at night OR
- co-danthramer with docusate (faecal softener) as co-danthrusate 50/60 1–3 capsules at night
- For patients with severe opioid-induced constipation, consider naloxegol 25 mg daily orally
- only prescribe on advice from the palliative care team
Symptoms relieved
- If patient taking opioids or with Parkinson's disease or multiple sclerosis, continue maintenance dose of the effective treatment daily indefinitely
- If patient not taking opioids, neither has Parkinson's disease multiple sclerosis, further treatment is individual to each patient
Symptoms not relieved
- If patient does not respond to the above medications or 2 of them in combination, consider macrogols again
© 2022 The Bedside Clinical Guidelines Partnership.
Created by University Hospital North Midlands and Keele University School of Computing and Mathematics.
Research and development team: James Mitchell, Ed de Quincey, Charles Pantin, Naveed Mustfa