Door-to-needle time’ should not exceed 1 hr
- Interval between patient's arrival and commencement of lumbar puncture (if indicated) and antimicrobial treatment (‘door-to-needle time’) should not exceed 1hr
- If bacterial meningitis strongly suspected, contact a consultant in infectious diseases
RECOGNITION AND ASSESSMENT
Symptoms and signs
- Headache, neck stiffness, photophobia
- Fever
- Impaired consciousness, coma and fits
- Clinical features of septicaemia or severe sepsis
Alert
- In the elderly, confusion can occur as the only symptom of meningitis in the absence of meningism or even of fever
Life-threatening features
- Altered consciousness
- Focal neurological deficit
- Raised intracranial pressure
- Convulsions
- Concurrent evidence of sepsis
Differential diagnosis
- Subarachnoid haemorrhage
- Other intracranial sepsis
- Systemic sepsis
- Other causes of confusion or of raised intracranial pressure
- Encephalitis
- look for symptoms of confusion, seizures, dysphasia or reduced conscious level
- Malaria in travellers
INITIAL MANAGEMENT
Penicillin Allergy
- True penicillin allergy is rare
- Ask the patient and record what happened when they were given penicillin
- If any doubt about whether patient is truly allergic to penicillin, seek advice from a microbiologist or consultant in infectious diseases
Only accept penicillin allergy as genuine hypersensitivity if convincing history of either rash within 72 hr of dose or anaphylactic reaction
Infection Control alerts
- Check for IC alert.
- If IC alert not available, check previous 12 months of microbiology reports
- If MRSA present, treat as tagged for MRSA. See MRSA management
- If ESBL, MGNB, CARB present, treat as tagged for ESBL. See ESBL/MGNB/CARB management
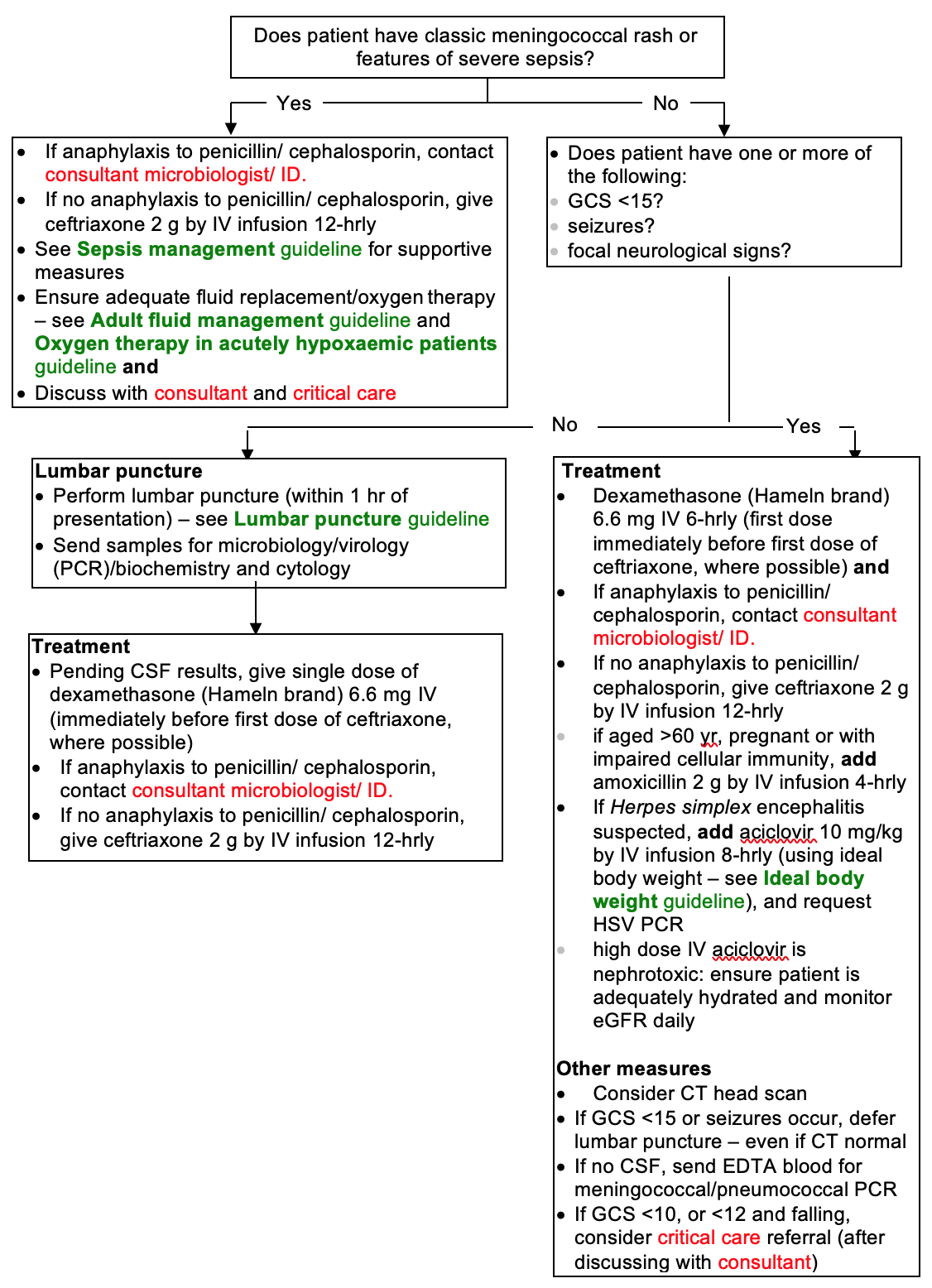
Immediate management
Immediate management tool
Investigations
- CSF
- if there are no clinical contraindications, perform lumbar puncture immediately. See Lumbar puncture guideline
- if there are no clinical contraindications to LP, CT scan is not indicated
- FBC, differential WBC and coagulation screen
- U&E, glucose and CRP
- Chest X-ray
Microbiology
- Throat swab (Include suspected meningococcal meningitis in clinical details. Take separate swabs for MRSA screening)
- Blood culture
- Meningococcal/pneumococcal PCR (EDTA tube)
- Urinary pneumococcal antigen
CSF results
CSF acellular
- Stop antimicrobials and corticosteroids and seek alternative diagnosis
CSF shows neutrophil predominance
- Continue dexamethasone (Hameln brand) 3.3 mg IV or 4 mg oral 6-hrly
- Continue antimicrobials
- if anaphylaxis to penicillin/ cephalosporin, contact consultant microbiologist/ ID
- if no anaphylaxis to penicillin/ cephalosporin, continue ceftriaxone 2 g by IV infusion 12-hrly. If aged >60 yr, pregnant or with impaired cellular immunity, add amoxicillin 2 g by IV infusion 4-hrly
CSF shows lymphocyte predominance
- Consider stopping antimicrobials and dexamethasone
- Consider other diagnoses (e.g. viral meningitis, tuberculous meningitis). Discuss with consultant +/- infectious disease team
Notification
- Notify cases of suspected community-acquired meningitis immediately to consultant in communicable disease control to discuss need for prevention of secondary cases
MONITORING TREATMENT
- Neurological observations, including GCS, every 15 min in severe cases initially, then at decreasing intervals as recovers
SUBSEQUENT MANAGEMENT
- If bacterial meningitis proven or probable, continue antimicrobial treatment for 7 days, then review
- if meningococci isolated, treat for 7 days, then review
- if pneumococci isolated, treat for 14 days, then review
- if other organisms isolated contact consultant microbiologist/ ID
- Withdraw dexamethasone after 48 hr unless specific indication to continue (e.g. TB meningitis)
- If encephalitis is not/no longer suspected, it is not necessary to continue aciclovir until a negative HSV PCR test result has been received
DISCHARGE AND FOLLOW-UP
- Follow-up in clinic to check for hearing loss
- Refer patients with persisting neurological deficit to appropriate specialist for rehabilitation:
- aged <65 yr – rehabilitation department
- aged ≥65 yr – consultant geriatrician linked to medical firm
© 2022 The Bedside Clinical Guidelines Partnership.
Created by University Hospital North Midlands and Keele University School of Computing and Mathematics.
Research and development team: James Mitchell, Ed de Quincey, Charles Pantin, Naveed Mustfa