RECOGNITION AND ASSESSMENT
Symptoms and signs
- >1 watery, loose or unformed stools within 24 hr
- ± signs of colitis
Risk factors
- Gastric acid suppression
- Advanced age,
- Prior hospitalisation,
- Duration of hospitalisation
- Care home residency
- Abdominal surgery
- Nasogastric tube
INITIAL MANAGEMENT
Laxative or antibiotic treatment
- If the diarrhoea may be caused by laxative or antibiotic
- stop laxative and, if possible, stop antibiotics
- for 24 hr follow impact on diarrhoea
- If the diarrhoea stops, do not submit a stool sample
- If the diarrhoea continues, send diarrhoeal stool sample
New unexplained diarrhoea
- Isolate patient with in a side room (any ward) within 2 hr
- Send diarrhoeal stool sample .
- If necessary, promptly escalate to site manager
Investigations
- FBC for WBC↑
- U&E
Stool sample for microbiology
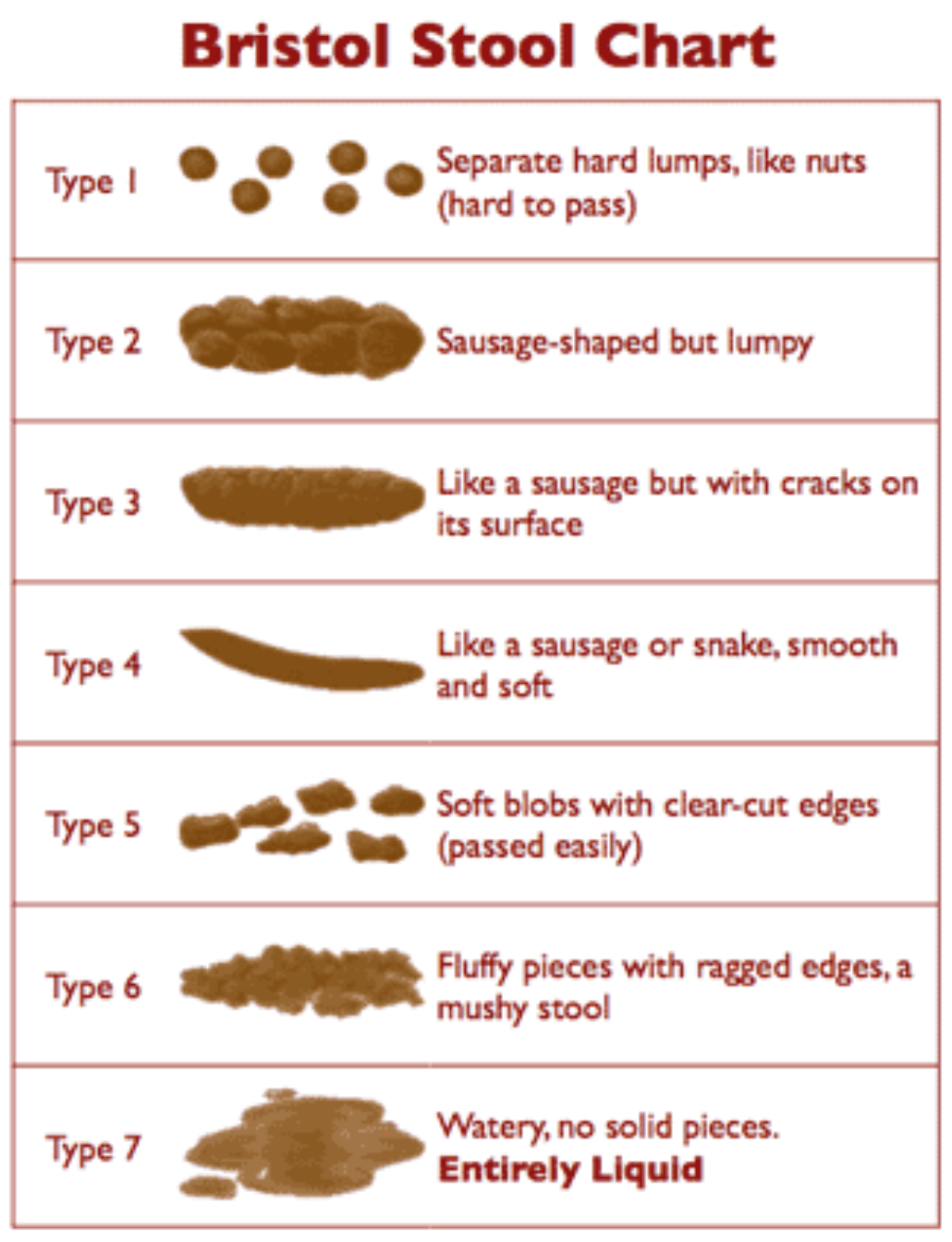
- A diarrhoeal sample is a stool taking the shape of the container
- The laboratory will not test formed stool
- Interpretation is provided with all test reports
Colitis
- Signs of colitis: X-rays/CT scan abdomen
- Lower gastrointestinal endoscopy for tissue biopsy
- invasive
- in severe colitis may increase the risk of perforation
- in case of doubt about diagnosis, contact gastroenterologist
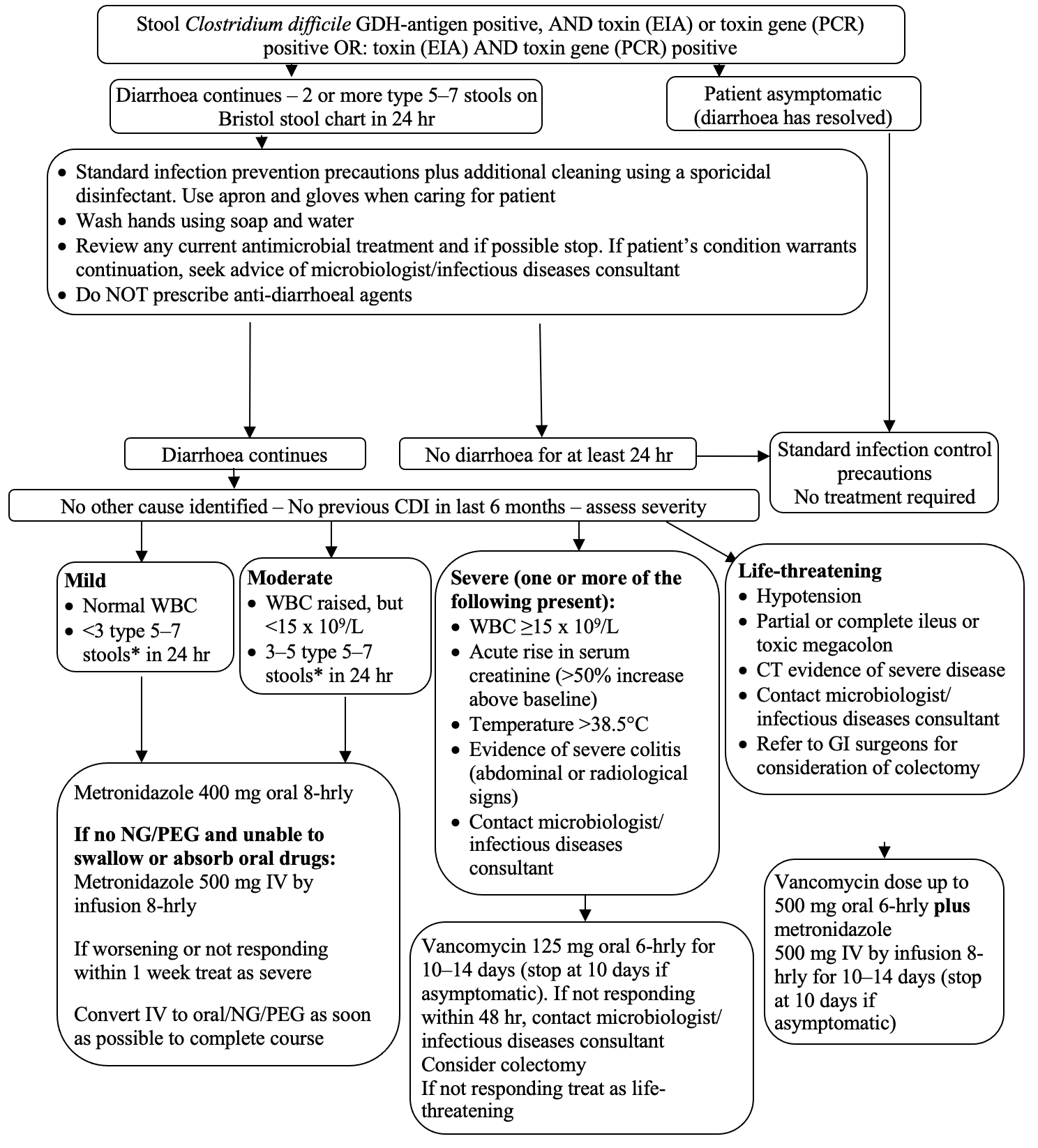
CONFIRMED CDI MANAGEMENT
- Confirmed=Stool C. difficile GDHA positive with TEIA or PCRG positive
Management
- Nurse in single room (any ward)/C. difficile cohort ward
- Contact infection prevention team (IPT)
- Avoid successive uninterrupted courses of different antimicrobials for any indication
Treatment tool
SUBSEQUENT MANAGEMENT
- Nurse patient in side room/cohort ward until symptom-free for 72 hr
- If another cause identified, discuss with microbiologist/ID consultant
- If mild/moderate CDI deteriorates, or if diarrhoea fails to respond to antimicrobial treatment of CDI for>5 days, discuss with microbiologist/ ID consultant
Repeat stool samples
- Unless diagnosis in doubt, do not send repeat stool within 72 hr
- If GDHA and TEIA positive, do not send further stool for CDI testing within 28 days
- stool can remain toxin positive for several weeks
Recurrence/non-responder
- Keep in side-room irrespective of symptoms until the first of:
- hospital discharge or
- 6 months have elapsed since last CDI diagnosis
- Review any current antimicrobial treatment and if possible, stop
- If life-threatening colitis, refer to GI surgeons for consideration of colectomy
- First recurrence within 6 months, or if no response to oral vancomycin within 2–5 days:
- treat with fidaxomicin 200 mg 12-hrly for 10 days
- Subsequent recurrence within 6 months (3rd or further episode of CDI):
- consider HPI
- otherwise, commence fidaxomicin 200 mg 12-hrly, to be given for 10 days
Faecal Microbiota Transplant (FMT) Infusion
- Infusion of a filtrate of gut flora derived from healthy donor faeces
- Patients with recurrent CDI treated with HPI demonstrated:
- 91% primary cure rate with symptoms usually resolving within 48 hr
- reduced risk of recurrent CDI in the following months provided that the patient does not receive further antibiotics
- Consider HPI for a 3rd or further episode of CDI
Administration
- Obtain patient’s consent
- Contact microbiologist
- Complete HPI order form for microbiologist to order from the PHE laboratory
- Preparation of stool from pre-screened universal donors will arrive in 3–4 days
- Stop all antibiotic treatment (including for CDI) on the day before HPI is to be administered
- Prepare patient for administration
- via nasogastric, naso-jejunal tube or PEG,
- if other routes are not an option, via colonic infusion by a gastroenterologist