RECOGNITION
- Vitamin deficiency usually develops slowly over several months to years
- Vitamin deficiency signs and symptoms may be subtle at first
- increase as the deficiency worsens
Symptoms
Neurological
- Numbness or paraesthesia
- Muscle weakness
- Unsteady movements
Megaloblastic anaemia
- Breathlessness
- Fatigue
- Dizziness
Non-specific
- Memory loss
- Personality changes
- Mental confusion or forgetfulness
- Irregular heartbeats
Signs
- Pale or yellowish skin
- Glossitis
- Peripheral neuropathy
- especially proprioception
- Sub-acute combined degeneration of the cord
- which may occur in the absence of anaemia
Assessment
- Diet
- Features of malabsorption
- Personal/FH of autoimmune conditions
- GI surgery
- Medication use
- e.g. proton pump inhibitors, metformin, OCP
- Pregnancy and OCP
- oestrogen reduces serum B12 (but not functional B12)
- by 25% on oral contraceptive pill
- by <30% by third trimester of pregnancy
- level >150 pg/mL may therefore be normal
Investigations
- FBC
- Folate
- Serum cobalamin (B12)
- Anti-intrinsic factor Ab (anti-IF Ab)
- if suspect PA, test for anti-IFAB regardless of cobalamin levels
INITIAL MANAGEMENT
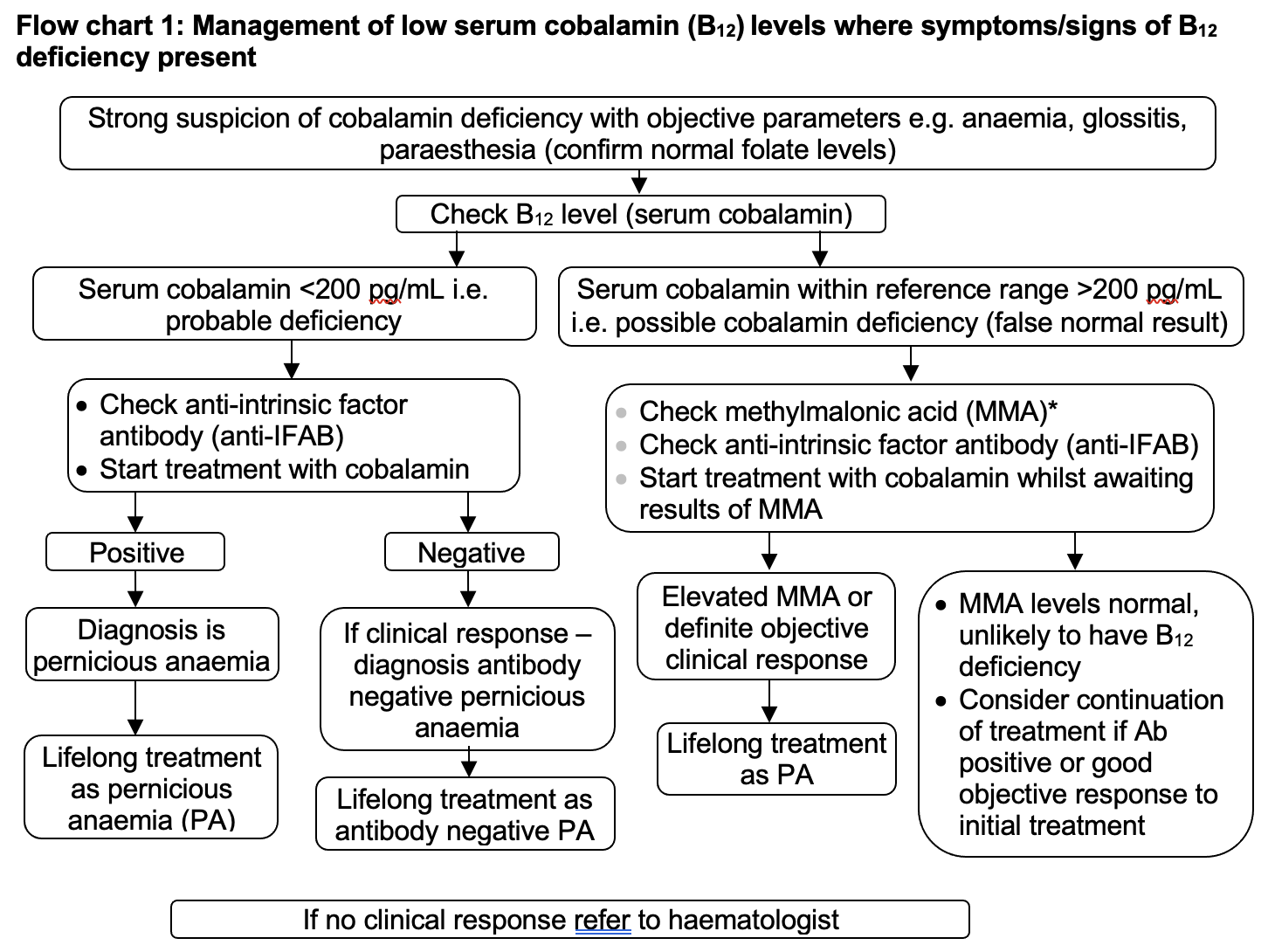
Symptoms/signs of B12 deficiency present
Management of low serum cobalamin (B12) levels where symptoms/signs of B12 deficiency present
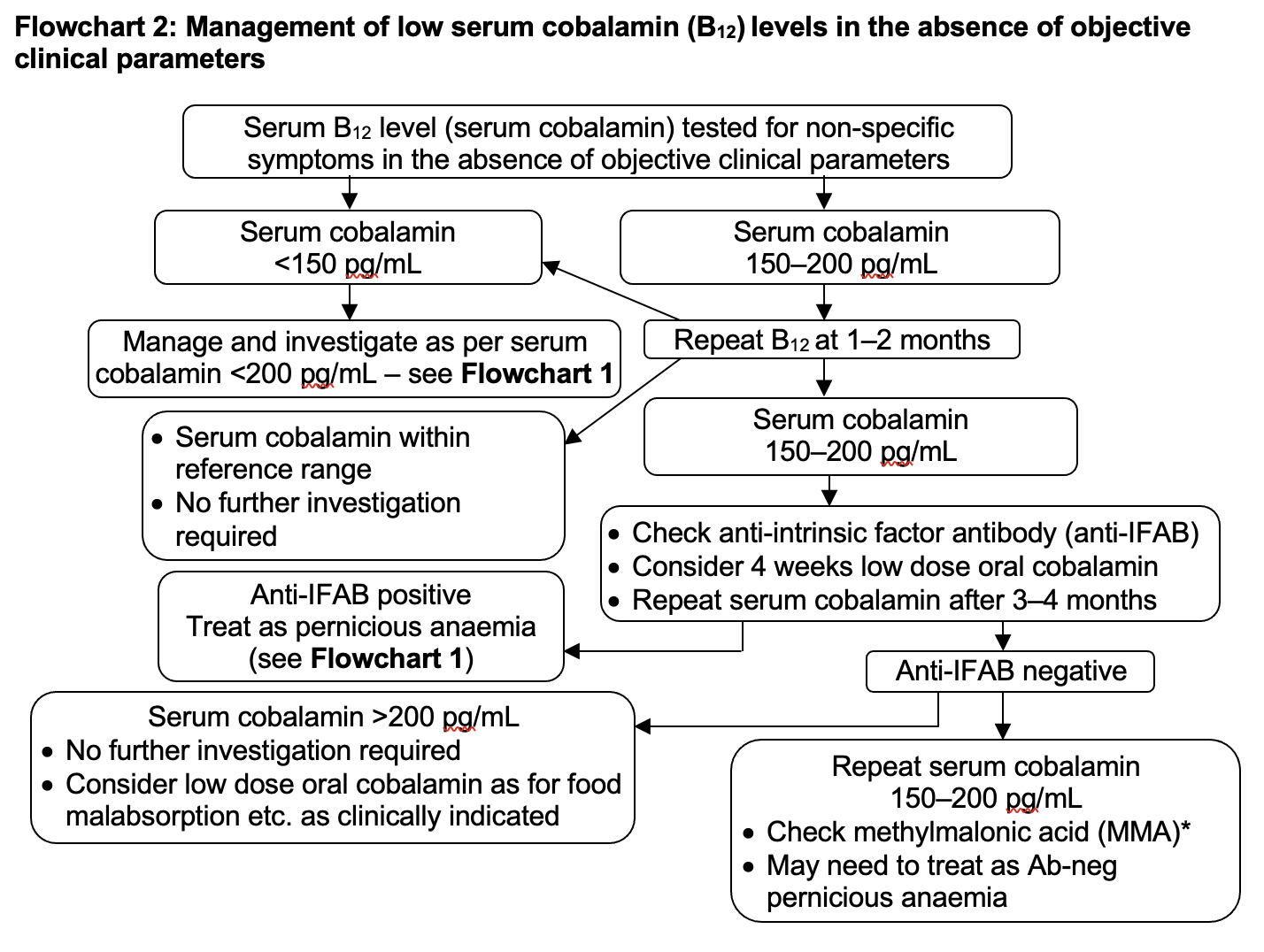
B12 low but symptoms/signs absent
- B12 ≤ 200 pg/mL
- Non-specific symptoms
Management of low serum cobalamin (B12) levels in the absence of objective clinical parameters
TREATMENT
Pernicious anaemia
- Prescribe vitamin B12 as hydroxocobalamin
- Treatment regimens are dependent on symptoms/signs. See BNF
Dietary cause
- Dietary sources of B12 include eggs, milk/dairy products, salmon, fortified products e.g. cereals
- In the absence of neuropathy, consider oral cyanocobalamin 50–250 microgram daily taken between meals (although higher doses <2000 mg may be required)
- check B12 levels at 1–3 months
- Duration of B12 supplementation depends on the cause of the deficiency and response
- When using oral cyanocobalamin, caution regarding possible emerging pernicious anaemia
RBC transfusion in chronic anaemia
- Consider a single unit RBC transfusion in patients with:
- moderate/severe symptoms
- haemodynamically stable
- reversible cause of anaemia
- Hb <90 g/L
- Remember each unit transfused is a treatment decision
- See Chronic Anaemia: RBC transfusion
ASSESSING RESPONSE
- If patient receiving IM hydroxocobalamin, do not routinely check B12 levels
- Monitor for hypokalaemia after commencing B12 replacement and consider replacement
- If PA, assess reticulocyte response at 7–10 days
- suboptimal response may indicate concomitant iron deficiency
DISCHARGE
- Inform GP of:
- cause
- treatment
- monitoring required
© 2022 The Bedside Clinical Guidelines Partnership.
Created by University Hospital North Midlands and Keele University School of Computing and Mathematics.
Research and development team: James Mitchell, Ed de Quincey, Charles Pantin, Naveed Mustfa