RECOGNITION AND ASSESSMENT
- Untreated, it carries a 15% mortality rate
- Occur as a presenting feature
- Occur as an unexplained development in a patient who has been admitted for other reasons and deprived of alcohol
- if frequent attendance at hospital (e.g. upper GI symptoms), pay particular attention
- Intoxicated patients with a high degree of tolerance towards alcohol may develop alcohol withdrawal symptoms
- even while their alcohol level may still seem high
- Mild withdrawal generally begins 6–8 hr after last drink, but can be sooner or considerably delayed
- Moderate-severe withdrawal occurs about 48 hr after last drink
Symptoms and signs
- Anxiety
- Sweating
- Tremor
- Ataxia
- Confusion
Assess severity
- Assess vital signs and record on NEWS chart
- Assess severity with Clinical Institute Withdrawal Assessment of Alcohol Scale (revised CIWA-Ar) form
- for advice on assessment, contact alcohol liaison nurse
- use CIWA-Ar in management below
Alcohol history
- Complete Alcohol screening tool (AUDIT)
- Quantity, frequency and highest daily alcohol use
- Previous treatment for alcohol misuse
- Previous abstinence
- Triggers for drinking
- Psychiatric problems
- Motivation
Investigations
Routine
- If decompensated alcoholic liver disease (ascites, encephalopathy) or a GI bleed, blood cultures
- FBC
- U&E
- LFT
- INR
- Bone profile plus magnesium and phosphate
- Blood glucose
Optional
- If severe withdrawal or severe systemic upset, arterial blood gases
- if illicit drug use suspected, urine drugs of abuse screen
- some of the newer drugs (‘legal highs’) may be difficult to identify
- Breath/blood alcohol
- Gamma-glutamyl transpeptidase test (GGT)
Differential diagnosis
- See Delirium (acute confusional state) in older people guideline
- Acute alcoholic hepatitis with hepatic encephalopathy
- Withdrawal of intoxication with drug(s) of misuse. See Withdrawal of drug(s) of dependence guideline
Alcohol related brain damage (ARBD)
- Alcohol related brain damage (ARBD) is an umbrella term
- spectrum of brain disorder including alcohol related dementia, alcohol amnesic syndrome and Wernicke-Korsakoff’s syndrome
- if left untreated can lead to irreversible brain damage, disorders of the nervous system and death
- If patient presents to ED appearing intoxicated, confused, ‘off legs’, consider ARBD
- Diagnosis is supported by the presence of the following:
- alcohol related hepatic, pancreatic, gastro-intestinal, cardiovascular or renal damage
- ataxia or peripheral neuropathy
- evidence on neuro imaging of brain atrophy
IMMEDIATE MANAGEMENT
- The aim is to prevent features of withdrawal without over sedation
- If there is suspicion or evidence of alcohol dependence, monitor
Alcohol withdrawal in pregnancy
- Commence CIWA-Ar symptom assessment
- Discuss with alcohol liaison team, substance misuse midwife and alcohol management unit regarding tapered reduction of benzodiazepines
Monitor
- Check conscious levels, respiratory status and alcohol withdrawal symptoms
- look for other organic pathology
- If drowsy, confused or there is concern about previous readings, blood glucose 2-hrly
- Record CIWA-Ar score hourly for 8 hr (all patients)
- if CIWA-Ar score <8 on 2 consecutive readings, reduce assessments to 2-hrly. Continue for next 8 hr
- if CIWA-Ar score ≥8 on any reading, return to hourly assessments
- After 8 hours, if CIWA-Ar score <8 and not rising, reduce assessments to 4-hrly for next 48 hr
- then stop assessment unless CIWA-Ar score ≥8
Which sedative?
- Lorazepam and diazepam normally given orally
- Prescribe diazepam unless:
- patient is frail elderly, diazepam intolerant, showing signs of delirium tremens, in respiratory failure or severe liver impairment (e.g. INR >2 and bilirubin >200 or hepatic encephalopathy), then use lorazepam
- If patient usually on a regular benzodiazepine e.g. temazepam 10 mg at night, continue this with additional diazepam or lorazepam prescribed as required to manage alcohol withdrawal symptoms
Dose of sedative
- Administer as required medication as directed by CIWA-Ar assessments
- record doses given on drug chart and CIWA-Ar chart
- Individual dose requirements vary considerably
- decide only by monitoring and omitting or adding doses as necessary
CIWA-Ar score ≥16 on monitoring
- 10 mg diazepam or 1 mg lorazepam
- if severe withdrawal symptoms, some patients may require higher than BNF recommended limits of benzodiazepines
CIWA-Ar score 10-15 on monitoring
- 5 mg diazepam or 0.5 mg lorazepam
CIWA-Ar score <10 on monitoring
- No need for withdrawal medication
Parenteral thiamine
- Most effective when given parenterally as oral absorption is poor
- Prefer IV route but if not available, use IM route
- Give Pabrinex IV high potency injection 2 pairs of ampoules (mixed) by IV infusion in sodium chloride 0.9% 100 mL over 30 min 8-hrly
- if IV route not available, give 1 pair of ampoules deep IM into gluteal muscle 12-hrly. Use Pabrinex preparation specific to IM injections
Treatment duration
- If decompensated liver disease, malnourishment/significant weight loss, memory disturbance, risk of Wernicke’s encephalopathy, continue Pabrinex for 72 hr
- If Wernicke’s encephalopathy is suspected or confirmed and physical symptoms persist beyond 72 hr but patient is improving symptomatically, give 1 pair of ampoules IV or deep IM once daily for as long as symptoms continue to improve for a minimum of 5 days
- In all other patients 72 hr of Pabrinex is not essential
- e.g. if patient medically fit for discharge within this time, do not continue
Fluids and electrolytes
- Monitor and replace electrolytes, magnesium and phosphate
- Give adequate hydration. See Adult fluid management guideline
- defer glucose infusions until after first dose of Pabrinex given as it can precipitate Wernicke’s encephalopathy
Criteria to discuss with senior medical staff
- Patient has required 3 mg lorazepam or 30 mg diazepam over 3 hr
- CIWA-Ar score >35
- Evidence of Delirium Tremens, a medical emergency
Referral
- If patient scores 11–12 on AUDIT-C or requires CIWA-Ar monitoring, refer to alcohol liaison team
Admission criteria
- Confusion or hallucinations
- Epilepsy or history of fits
- Undernourished
- Severe vomiting or diarrhoea
- Uncontrollable withdrawal symptoms
- Acute physical illness requiring admission
- Decompensated liver disease
Critical care discussion
- Total dose of lorazepam has reached 8 mg and patient still agitated
- Respiratory depression
- Patient in state of extreme agitation
Not for admission
- Advise patient to avoid sudden reduction in alcohol intake
- Refer to alcohol liaison team or give information on local alcohol support services
- Give a dose of Pabrinex IV as per guidance
- If the patient is observed in the ED, continue Pabrinex IV 8-hrly
SUBSEQUENT MANAGEMENT
Reassess patient
- If withdrawals persist, consider changing from diazepam to lorazepam
- If unable to tolerate oral benzodiazepines, or symptoms of severe hallucinations or agitation, consider use of parenteral lorazepam 1 mg (preferably IV into a large vein) with interval between doses of at least 15 min (IV) and 30 min (IM)
- do not use IM route in patients with bleeding/clotting disorders
- Haloperidol 1–5 mg can be added to enhance sedative effects of benzodiazepines
- see BNF for contraindications
Seizures
- Manage seizures, see First seizure guideline and Cluster seizures guideline
- However, withdrawal seizures alone do not signify epilepsy and maintenance anticonvulsant therapy is unnecessary
DISCHARGE AND FOLLOW-UP
- Where possible, liaise with alcohol liaison nurses to plan discharge
- Ensure all patients have been assessed for alcohol dependency with the AUDIT alcohol screening tool
Screening results (AUDIT score)
- <8: no action required
- 8–19: advice and offer referral to community alcohol services
- 20+: refer to alcohol liaison nurse
Drugs on discharge
- Prescribe oral thiamine 100 mg 8-hrly for all patients on discharge
- advise GP via discharge letter to continue this for 3 months in the community
- Do not start discharged patients on vitamin B compound
- in those admitted on vitamin B solely for the reason of alcohol dependency stop unless malnourished
- If patient malnourished refer to dietitian and discuss need for ongoing vitamin supplementation
- Alcohol liaison team may advise prescribing Acamprosate:
- body weight ≥60 kg – 666 mg 8-hrly
- body weight <60 kg – 666 mg at breakfast, 333 mg at midday and 333 mg at night
- to be continued on discharge and reviewed by GP or community alcohol service
Driving
- Advise patient to contact the DVLA and car insurance provider
- with alcohol related illness, they should not drive for 6 months
- with alcohol withdrawal, they should not drive for 12 months
CIWA-Ar
Select one of each domain
Nausea/vomiting
Ask: “Do you feel nauseated? Have you vomited? Rate on scale 0-7
Tremor
Have patient extend arms & spread fingers. Rate on scale 0 - 7
Anxiety
Ask: Do you feel anxious? Rate on scale 0 – 7
Agitation
Observe patient. Rate on scale 1-7
Paroxysmal sweats
Observe patient - Rate on Scale 0 - 7
Orientation and clouding of sensorium
Ask, “What day is this? Where are you? Who am I?” Rate scale 0 - 4
Tactile disturbances
Ask, “Have you experienced any itching, pins & needles sensation, burning or numbness, or a feeling of bugs crawling on or under your skin?”
Auditory Disturbances
Ask, "Are you more aware of sounds around you? Are they harsh? Do they startle you? Do you hear anything that disturbs you or that you know isn’t there?”
Visual disturbances
Ask, “Does the light appear to be too bright? Is its colour different than normal? Does it hurt your eyes? Are you seeing anything that disturbs you or that you know isn’t there?”
Headache
Ask, “Does your head feel different than usual? Does it feel like there is a band around your head?” Do not rate dizziness or light-headedness"
Alcohol screening tool (Audit)
Select one of each domain
Often drinks alcohol
Ask: How often do you have a drink containing alcohol?
Drinks on a typical day (units of alcohol)
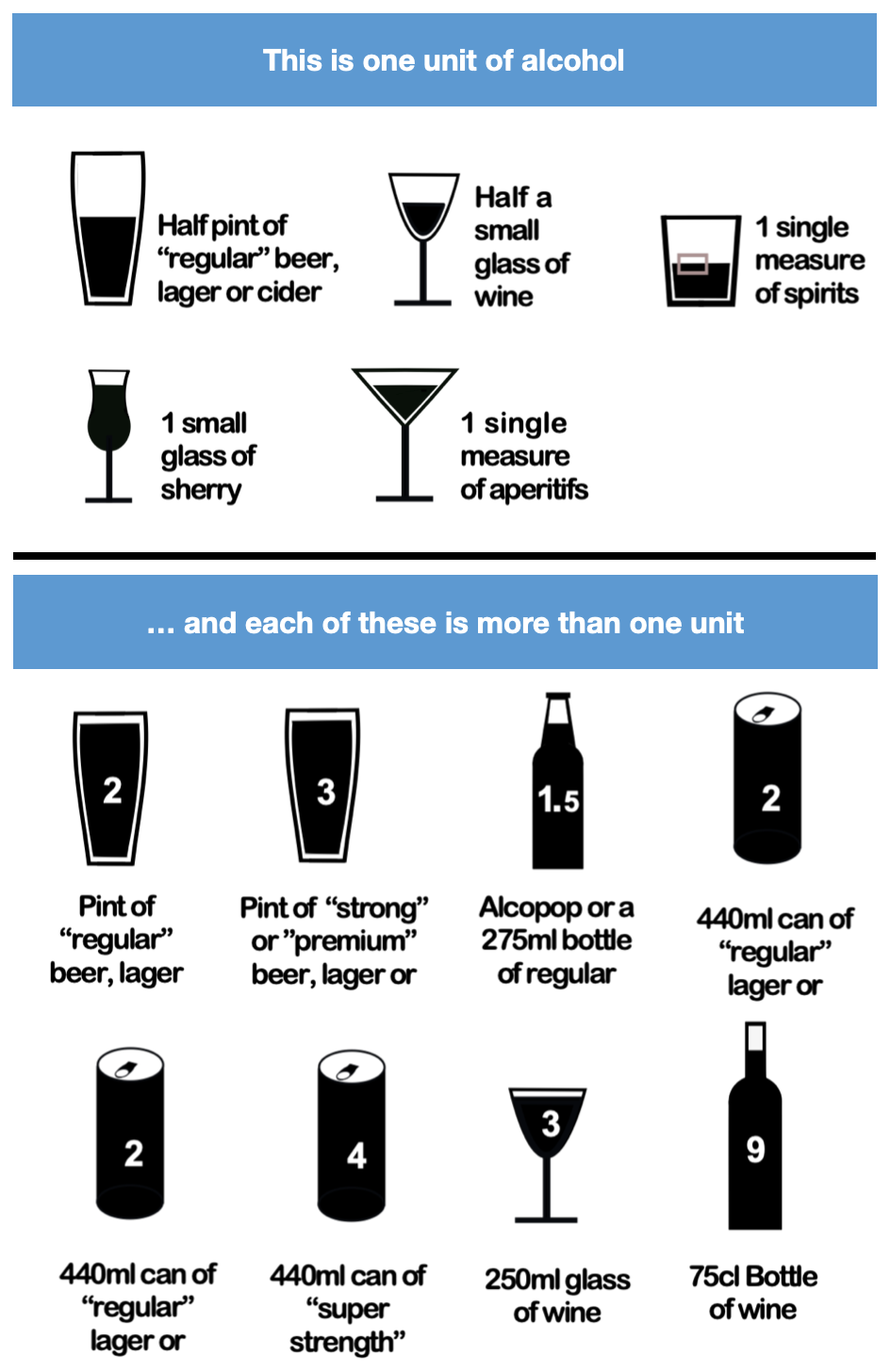
Ask: How many units of alcohol do you drink on a typical day when you are drinking?
Units of Alcohol
Ask: How often have you had 6 or more units if female, or 8 or more if male, on a single occasion in the last year?
Not able to stop drinking once started
Ask: During the last year have you found that you were not able to stop drinking once you had started?
Failed to do what was normally expected because of drinking
Observe patient - Rate on Scale 0 - 7
Needed an alcoholic drink in the morning
Ask: How often during the last year have you needed an alcoholic drink in the morning to get yourself going after a heavy drinking session?
Had a feeling of guilt or remorse after drinking
Ask: How often during the last year have you had a feeling of guilt or remorse after drinking?
Unable to remember what happened the night before
Ask: How often during the last year have you been unable to remember what happened the night before because you had been drinking?
Somebody been injured as a result of your drinking?
Ask: Have you or somebody else been injured as a result of your drinking?
Others concerned about your drinking?
Ask, "Has a relative or friend, doctor or other health worker been concerned about your drinking or suggested that you cut down?"
© 2022 The Bedside Clinical Guidelines Partnership.
Created by University Hospital North Midlands and Keele University School of Computing and Mathematics.
Research and development team: James Mitchell, Ed de Quincey, Charles Pantin, Naveed Mustfa