RECOGNITION AND ASSESSMENT
- Anaphylaxis is a severe systemic allergic reaction
- Consider if rapid onset of respiratory difficulty and/or hypotension
- especially if rash and/or angioedema present
Symptoms and signs
Airway
- Upper airways obstruction due to angioedema:
- swelling of tongue/throat
- stridor
- feeling of throat closing
- hoarse voice
Breathing
- Lower airways obstruction:
- wheeze
- increased respiratory rate
- cyanosis
Circulation
- Signs of shock:
- impaired capillary refill (capillary refill time >2 sec)
- tachycardia
- hypotension
Disability
- Confusion
- Agitation
- Loss of consciousness
Exposure
- Skin and mucosal changes (may not be present in all patients):
- redness or blotchy rash
- urticaria
- itching
- angioedema
- rhinitis and conjunctivitis
Other systems affected
- Gastrointestinal:
- abdominal pain
- vomiting
- diarrhoea
Investigations
- Mast cell tryptase – sample serum at following times
- as soon as possible after emergency treatment has started
- at 1–2 hr from onset of symptoms. No later than 4 hr
- Patient may present late. Take as many serum samples as time since presentation allows
- indicate time and date clearly to allow interpretation of results
- Inform patient that a final sample will be necessary to measure baseline levels in follow-up
Differential diagnosis
- Syncope (rapid recovery) with bradycardia in vagal reaction
- Septic shock with a petechial or purpuric rash
- Acute cardiac event
- Panic attack with hyperventilation (unlikely to be hypotensive)
- Acute severe asthma
- Other causes of central airways obstruction
- idiopathic non-allergic urticaria and angioedema
IMMEDIATE MANAGEMENT
- All doses are for adults
Diagnosis
Look for
- Acute onset of illness
- Life-threatening Airway and/or Breathing, and/or Circulation problems
- Airway: Swelling, hoarseness, stridor
- Breathing: Rapid breathing, wheeze, fatigue, cyanosis, SpO2 <92%, confusion
- Circulation: Blotchy and red, clammy, low blood pressure, faintness, drowsy/coma
- Usually skin changes
Call for help
- Lay patient flat and elevate feet to restore/maintain BP. Do not stand patient up
- if this causes respiratory distress, sit patient up
Adrenaline
- For hypotension or respiratory distress with stridor or wheezing, give adrenaline:
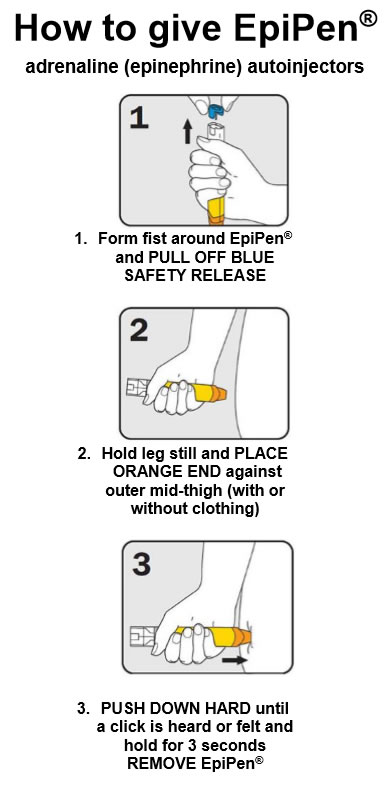
- 500 microgram (0.5 mL of 1:1000 solution) IM into midpoint of anterolateral aspect of thigh
- if an adult EpiPen® is more readily available give this (delivers 300 microgram dose of adrenaline)
- If hypotension and respiratory distress do not respond within 5 min:
- give further dose of adrenaline 500 microgram IM (0.5 mL of 1:1000 solution)
- Can be repeated at 5 min intervals according to BP, heart rate and respiratory function
- monitor vital signs continuously
- IV adrenaline is hazardous
- use only with extreme care, and under critical care supervision, for those in profound shock that is immediately life-threatening
When skills and equipment available
Establish airway
- If concerned about patient’s respiratory effort/airway obstruction, contact anaesthetist
High-flow oxygen
- Oxygen at high flow rate (10–15 L/min) – see Oxygen therapy in acutely hypoxaemic patient guideline
IV fluid challenge
- Establish IV access
- If systolic BP <100 mmHg, give fluid challenge of compound sodium lactate (Hartmann’s) 500 mL as quickly as possible. See Fluid resuscitation guideline
- Stop IV colloid if this might be cause of anaphylaxis
Chlorphenamine
- Chlorphenamine 10 mg by IM or slow IV injection
Bronchospasm
- If there is bronchospasm, give salbutamol 5 mg via oxygen driven nebuliser
- for further treatment of bronchospasm, see Acute severe asthma in adults guideline
- If patient has been taking a non-cardioselective beta-blocker [e.g. propranolol, oxprenolol, sotalol, timolol (including eye drops)], severity of anaphylaxis may be increased and response to adrenaline antagonised
- consider giving salbutamol by slow IV injection – see Salbutamol IV guideline
Severely ill patient
- When patient severely ill and there is real doubt about adequacy of circulation and absorption after IM injection, call critical care staff to attend urgently
- transfer to critical care as soon as possible
Further treatment under critical care supervision
- Consider giving adrenaline 50 microgram (0.5 mL of the dilute 1:10,000 adrenaline injection) by slow IV injection, no faster than 1 mL/min while monitoring cardiac rhythm.
- Repeat according to response
- If multiple doses required, give adrenaline as slow IV infusion, stopping when response obtained
MONITORING
- Monitor (including ECG) continuously all patients experiencing severe anaphylaxis until condition stabilised
- then every 15 min for 1 hr until completely stable
- Continue to record hourly:
- heart rate
- blood pressure
- respiratory rate
- if possible, peak expiratory flow (PEF)
- SpO2
SUBSEQUENT MANAGEMENT
- Record time of onset of symptoms and identify possible allergens
- e.g. drugs, foods (within previous hour), insect stings, latex
- Until all allergic symptoms have subsided completely, consider prednisolone 30 mg oral daily
- Chlorphenamine 4 mg oral 6-hrly (for at least 24–72 hr to prevent relapse) or until all allergic symptoms have subsided completely
- Warn patient of possible early recurrence and keep under observation for at least 6 hr.
- Consider prolonged observation for patients who:
- developed symptoms during night, who may not be able to respond to any deterioration in clinical condition
- live in areas where access to emergency care difficult
Likelihood of early recurrence
- Increased in patients:
- with slow-onset severe reaction resulting from idiopathic anaphylaxis
- with severe asthma
- at risk of continued absorption of allergen
- with previous history of biphasic reactions
DISCHARGE AND FOLLOW-UP
- Senior clinician reviews patient before discharge
- Patient given clear instructions to return to hospital if symptoms return
- Advise avoidance of allergen if appropriate
- Management plan to include use of antihistamines for any allergic symptoms and EpiPen® and 999 call for life-threatening symptoms of dyspnoea or faintness
- Prescribe 2 auto-injector devices containing adrenaline 300 microgram (EpiPen® )
- instruct patient on when and how to use
- Give patient contact details for SOS Talisman to obtain alert jewellery containing vital information on their condition in case of emergency
- Give patient contact details of Anaphylaxis Campaign,
- Send outpatient referral
© 2022 The Bedside Clinical Guidelines Partnership.
Created by University Hospital North Midlands and Keele University School of Computing and Mathematics.
Research and development team: James Mitchell, Ed de Quincey, Charles Pantin, Naveed Mustfa