RECOGNITION AND ASSESSMENT
- Acute coronary artery syndromes comprise myocardial infarction and unstable angina, and are currently distinguished by history, ECG and presence or absence of cardiac biomarkers of myocardial injury
Symptoms and signs
- Severe, persistent chest pain
- Dyspnoea
- Fear
- Pallor
- Sweating
- Anxiety
- Peripheral vasoconstriction
- Shock
Investigations
- ECG
- Locally available cardiac biomarkers of myocardial injury
- Raised cardiac biomarkers signify myocardial infarction, not unstable angina
- A raised troponin I concentration can suggest myocardial necrosis but can also occur in a number of other conditions:
- auto-immune disease
- congestive cardiac failure
- critical illness
- dilated cardiomyopathy
- extreme physical effort
- hypertension
- hypothyroidism
- multiple injury
- myocarditis
- pericarditis
- pneumonia
- pulmonary embolism
- renal failure
- sepsis/septic shock
- subarachnoid haemorrhage
- tachyarrythmias
- vasculitis
- Plasma cholesterol (within 12 hr of onset of symptoms; otherwise leave for at least 6 weeks)
- Venous blood glucose and HbA1c
- FBC, INR, APTT
IMMEDIATE TREATMENT
- Aspirin 300 mg (chew and swallow)
- Diamorphine 1 mg/min IV until pain relieved, up to maximum 10 mg (5 mg in elderly or frail patients)
- Metoclopramide 10 mg IV over 1–2 min (5 mg in young adults 15–19 yr <60 kg) with ≥8 hr before repeating
- Oxygen – see Oxygen therapy in acutely hypoxaemic patients guideline
- Bisoprolol 2.5 mg oral daily, unless contraindicated (e.g. decompensated heart failure, bradycardia)
- Atorvastatin 80 mg once daily for all acute coronary syndromes, unless history of CKD present. Start with atorvastatin 20 mg once daily if history of CKD
Admission
- Admit all patients with acute myocardial infarction (MI), or unstable angina with acute ST depression and/or raised troponin I to CCU under the care of duty consultant cardiologist Contact on-call cardiology SpR immediately for immediate transfer and treatment
- If ECG shows ST elevation MI (STEMI), follow Management of STEMI
- If patient has a Non-ST elevation MI (NSTEMI), follow Management of NSTEMI
MANAGEMENT OF STEMI
- Administer loading dose of aspirin (300 mg oral) if not already given, and either clopidogrel [600 mg oral (unlicensed dose)] or prasugrel (60 mg oral) immediately
- if age <75 yr, weight >60 kg, and no previous TIA/stroke or severe liver impairment, give prasugrel;
- if age >75 yr, weight <60 kg or previous stroke or TIA, give clopidogrel
- Usual strategy for STEMI management for patients presenting within hospital is primary angioplasty (pPCI)
- if decision is not for primary angioplasty, only give thrombolytic therapy if directed by on-call cardiology service – then follow Thrombolytic therapy (STEMI). Usually a contraindication for primary angioplasty is a contraindication for thrombolysis
MANAGEMENT OF NSTEMI
- Treatment of choice for most patients for NSTEMI is inpatient cardiac catheterisation with early revascularisation, either by percutaneous intervention (PCI) or CABG.
- patients unlikely to be suitable for an early invasive strategy because of frailty or multiple co-morbidities should have that decision made early and by an experienced clinician
- Prescribe fondaparinux 2.5 mg once daily by SC injection
- Give clopidogrel loading dose 300 mg oral [600 mg (unlicensed dose) in those who are unstable and likely to require catheter lab management within 24 hr]
- Risk of bleeding is increased in patients with low body weight (<50 kg), physiological frailty, severe liver or renal failure (eGFR <20 mL/min), thrombocytopenia or defective platelet function and following surgery, trauma or haemorrhagic stroke.
- Seek advice from appropriate team (e.g. cardiology, renal, liver or haematology)
NON-DIABETIC PATIENTS WITH BLOOD GLUCOSE >11 mmol/L AND ALL PATIENTS WITH DIABETES MELLITUS
- On admission, check blood glucose/HbA1c and, if blood glucose is >11 mmol/L, refer to locally approved guidance for management of hyperglycaemia in ACS patients
- In patients with diabetes/raised blood glucose, seek advice from endocrinologist/diabetes nurse specialist early
SUBSEQUENT MANAGEMENT
- Aspirin 75 mg oral daily (to be continued indefinitely) plus:
- if STEMI and treated by pPCI with no history of CVA or TIA or cerebral bleed, and age <75 yr and weight >60 kg, prasugrel 10 mg daily for 12 months
- otherwise clopidogrel 75 mg oral daily for 1 year
- Bisoprolol 2.5 mg oral daily, or atenolol 25 mg 12-hrly (to be titrated to maximum tolerated dosage and continued indefinitely)
- If no clinical suspicion of significant mitral/aortic stenosis or hypertrophic cardiomyopathy, plasma creatinine <300 μmol/L and there is no other contraindication to using ACE inhibitor, start ramipril – see Introduction of an angiotensin-converting enzyme (ACE) inhibitor. Check electrolytes on day 3–5. Increase titration rapidly to achieve a dose on discharge as near to 10 mg as achievable
- Check statin (atorvastatin) has been prescribed, subject to renal function
- give patient information sheet
- If pain persistent, consider glyceryl trinitrate (GTN) infusion (see Glyceryl trinitrate guideline) or further dose of atenolol 5 mg IV if heart rate >70 beats/min and systolic BP >100 mmHg
- If pain persists, contact duty cardiology team to facilitate transfer to ward /CCU
- Unless complications ensue, recommend early return to physical activity:
- mobilisation depends on revascularisation strategy, with early mobilisation and discharge by day 3 the norm post STEMI managed with an early invasive strategy
- Refer all patients to rehabilitation co-ordinator, who will arrange for assessment all suitable patients by cardiac rehabilitation team as soon as practically possible before discharge
- patients not wishing to join rehabilitation programme – provide appropriate dietary advice
- Refer all patients treated with glucose and insulin infusions to diabetes nurse specialist to distinguish diabetes from stress-induced hyperglycaemia
MONITORING TREATMENT
- Continuous ECG monitoring for 24–48 hr (longer if continuing instability or arrhythmia)
- Measure BP 4-hrly for 24 hr, then twice daily
- Daily 12-lead ECG. Plasma CK and AST on 2 consecutive days, unless troponin I already positive. If troponin is positive, no further cardiac enzyme assessments are warranted
- Observe for specific complications (more likely to occur if patient not re-perfused)
Specific complications
In all complications, seek further cardiological input
Arrhythmias
- See Cardiac arrhythmias
Pericarditis
- More likely after large infarcts
- Pain with persistent/intermittent pericardial rub 2–5 days after infarction
- Adequate analgesia (may need diamorphine). Give indometacin 25 mg oral 8-hrly if no contraindication (beware fluid retention and antagonism of loop diuretic)
Recurrent ischaemic pain
- Isosorbide mononitrate SR oral (GTN infusion if necessary – see Glyceryl trinitrate)
- If persistent chest pain occurs, refer to duty cardiology team for consideration of inpatient stress testing, coronary angiography and possible inpatient revascularisation
- If re-infarction occurs during admission, contact duty cardiology team immediately
Cardiac failure
- Advice in algorithm
Management of cardiac failure after acute MI
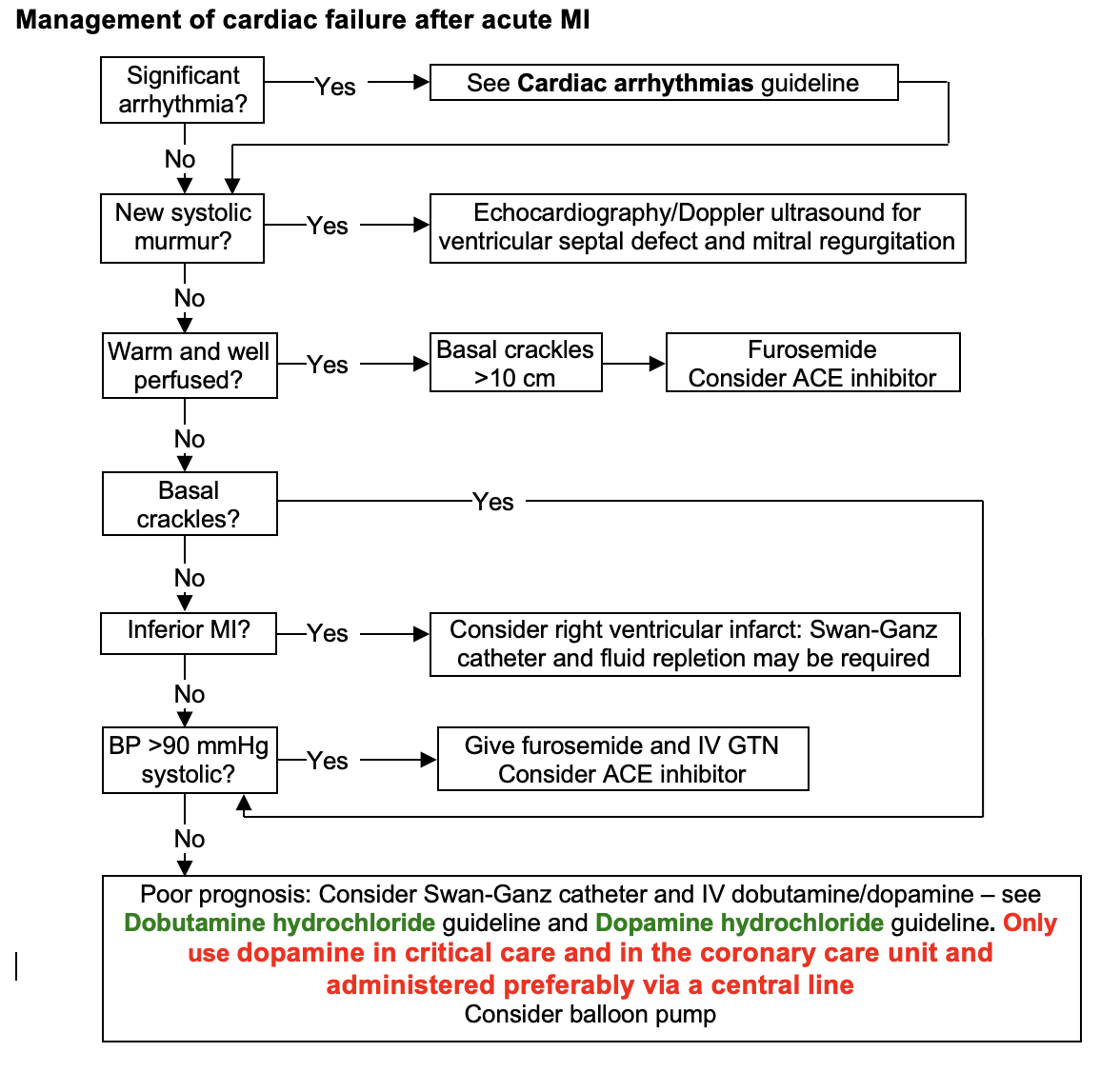
- In patients with left ventricular failure (LVF) or impaired LV function, introduce an ACE inhibitor as soon as this is practical – see Acute heart failure
- In patients with significant LVF and/or anterior Q wave infarct, arrange echocardiogram as outpatient, to document LV function and exclude LV aneurysm and/or thrombus
DISCHARGE AND FOLLOW-UP
- If no complications, discharge home on day 3–7
- Check risk factors for recurrent MI (e.g. smoking, hyperlipidaemia, hypertension, obesity) and advise or treat accordingly (mortality in first 2 years is doubled in those who continue to smoke and is 3.5-times greater if total cholesterol >6.5 mmol/L)
- Explain graded return to full activity (see advice booklet)
- Where appropriate, ensure patient has climbed stairs to assess for chest pain/shortness of breath
- Ensure advice booklet and chest pain alert card have been issued
- If taking atorvastatin, ensure GP letter regarding intensive statin therapy accompanies patient on discharge
- Warn about post-infarct angina
- Ensure GTN 400 microgram spray for sublingual use has been prescribed TTO and patient has been counselled on use
- Advise not to drive as per DVLA rules and check with insurer (Group 2 drivers must notify DVLA, taxi drivers must notify local council)
- Ensure referral has been made to cardiac rehabilitation team
- Check that rehabilitation plan has been made
- middle grade in cardiology will be able to review patients who attend as an outpatient at cardiac rehabilitation. Rehabilitation co-ordinator will arrange
- if patient declines cardiac rehabilitation or is unsuitable for programme, refer to cardiology follow-up clinic
- Check that follow-up has been arranged in diabetic clinic for all patients treated with glucose and insulin infusions
Follow-up clinic visit
- Ask about smoking, exercise and weight reduction
- Ask about angina – if occurring, consider referral for angiography
- Look for signs of heart failure and measure BP
- Check cholesterol
- If patient has not been to catheter laboratory, consider treadmill exercise
- Encourage return to work 1–3 months after infarction
- Resume driving 1 month after infarction (except Group 2 drivers)
- Unless there are contraindications, all patients should be taking the following treatment
STEMI
- ACE inhibitor (target dose ramipril 10 mg or equivalent)
- Statin therapy (target dose atorvastatin 80 mg or equivalent, unless history of CKD)
- Beta-blocker (target dose to achieve heart rate of 60 bpm at rest)
- Aspirin (75 mg) indefinitely
- If STEMI and treated by pPCI with no history of CVA or TIA or cerebral bleed, and age <75 yr and weight >60 kg, prasugrel 10 mg daily for 12 months
- otherwise clopidogrel 75 mg oral daily for 1 yr
NSTEMI
- ACE inhibitor (target dose ramipril 10 mg or equivalent)
- Statin therapy (target dose atorvastatin 80 mg or equivalent, unless history of CKD)
- Beta-blocker (target dose to achieve heart rate of 60 bpm at rest)
- Aspirin (75 mg) indefinitely
- Clopidogrel 75 mg oral daily for 1 yr
© 2022 The Bedside Clinical Guidelines Partnership.
Created by University Hospital North Midlands and Keele University School of Computing and Mathematics.
Research and development team: James Mitchell, Ed de Quincey, Charles Pantin, Naveed Mustfa